Understanding Protected Health Information and Its Examples
Protecting sensitive health data has become increasingly complex with the widespread use of electronic record-keeping in healthcare. As organizations rely more on digital platforms to manage patient information, it’s essential to understand what constitutes protected health information (PHI), how it is safeguarded, and the importance of compliance with regulations like HIPAA. This knowledge not only ensures patient confidentiality but also helps healthcare providers and organizations maintain trust and legal compliance.
Unlike traditional paper records, electronic health data requires sophisticated security measures to prevent unauthorized access, theft, or breaches. Recognizing what information qualifies as PHI, how it is stored, and the safeguards necessary to protect it is fundamental for anyone involved in healthcare management or policy.
What Does PHI Stand For in Healthcare?
The abbreviation PHI refers to protected health information, a term also associated with data regulated under HIPAA (the Health Insurance Portability and Accountability Act). This act mandates strict standards for safeguarding personal health details, ensuring that organizations handling such information maintain the highest levels of security and privacy. Understanding what constitutes PHI is crucial for healthcare providers, insurers, and administrators to remain compliant with federal regulations and to uphold patient rights.
What is PHI?
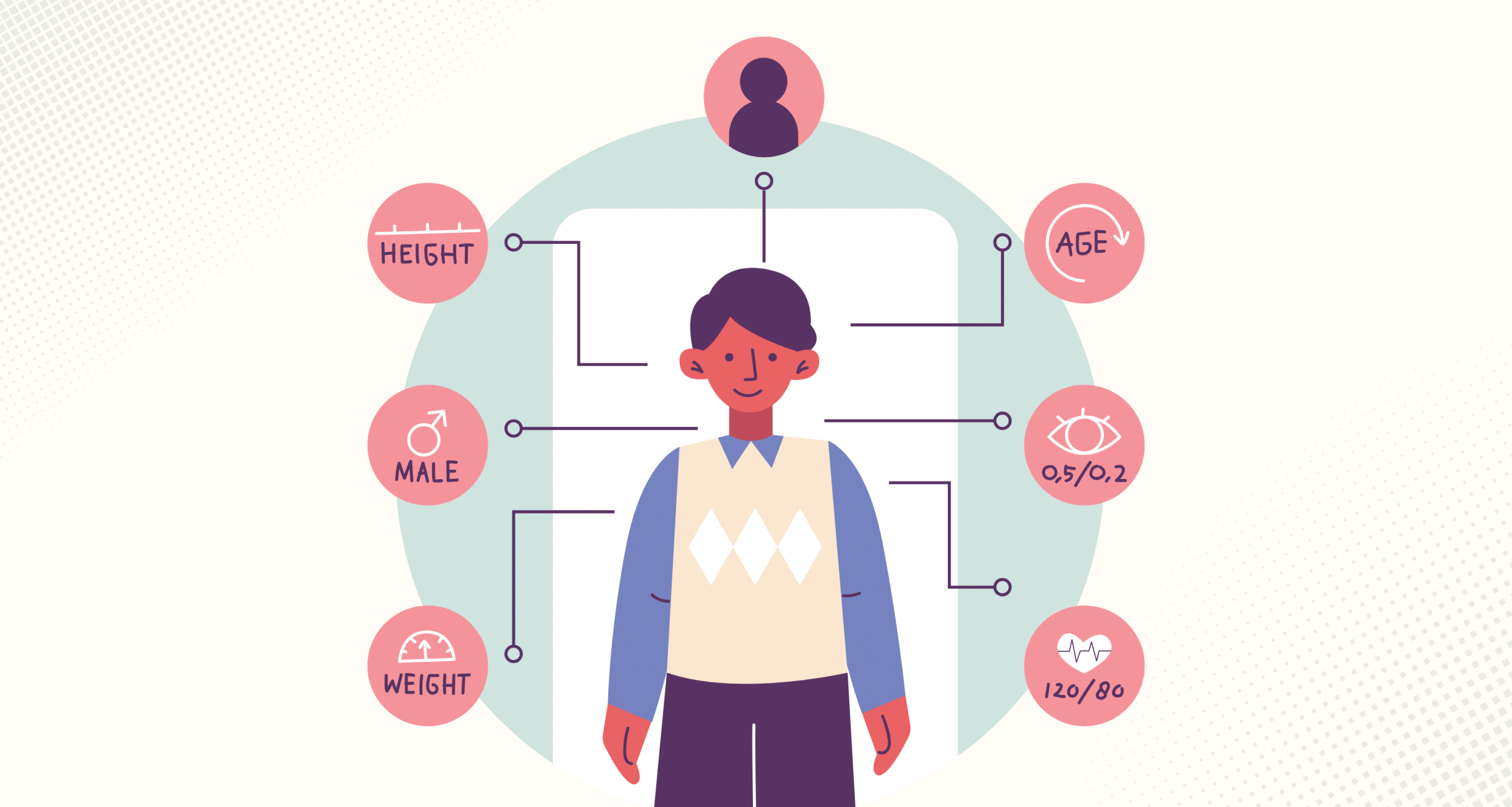
PHI encompasses any individual health-related data that can identify a person and was generated, used, or shared during medical diagnosis or treatment. This includes a broad range of information recorded throughout healthcare delivery and billing processes. The core principle is that any data which can directly or indirectly identify a patient, and is related to their health status or care, falls under the umbrella of PHI. Proper handling and protection of this information are vital, given its sensitive nature.
The Department of Health and Human Services (HHS) Office for Civil Rights (OCR) specifies 18 identifiers that, if associated with health information, qualify it as PHI. These identifiers range from personal details like names and addresses to biometric data and unique identification numbers. Recognizing these identifiers helps organizations implement appropriate security measures to ensure compliance and protect patient privacy.
Examples of PHI
- Full name
- Residential address, including street, city, county, or ZIP code (excluding broader geographic areas)
- Specific dates related to the individual, such as birth date, admission/discharge dates, or date of death, especially when not limited to just the year
- Contact details like telephone and fax numbers
- Email addresses
- Social Security numbers
- Medical record or account numbers
- Health plan beneficiary or insurance identifiers
- Unique certificates or license numbers
- Vehicle identifiers, serial numbers, or license plate details
- Device serial numbers or identifiers
- Web URLs and IP addresses
- Biometric data, such as fingerprints or voice prints
- Full-face photographs
- Any other unique identifiers or codes used to distinguish individuals
PHI and HIPAA
The HIPAA Privacy Rule establishes national standards to protect PHI held by covered entities such as healthcare providers, insurers, and clearinghouses. It grants patients rights over their health information and prescribes how organizations should handle and disclose PHI. The regulation emphasizes the importance of maintaining data confidentiality and integrity through strict policies and procedures.
To ensure the security of PHI, organizations must implement comprehensive safeguards across administrative, physical, and technical domains. Encryption is a critical security layer that ensures only authorized personnel can access sensitive data, often by requiring passwords or other authentication methods.
Interesting:
Additional safeguards include:
- Firewalls and intrusion detection systems
- Antivirus and anti-malware software
- Regular data backups
- Restricted access controls to limit data to essential personnel
Limiting access and enforcing policies for granting or revoking permissions are essential components of compliance. Employees should receive ongoing training on how to handle PHI securely, whether in hard copy or electronic form. This includes guidance on creating strong passwords and promptly reporting any data breaches, which helps maintain the integrity of health information.
What is ePHI?
Electronic protected health information (ePHI) refers to any PHI that is created, stored, transmitted, or received electronically. The HIPAA Security Rule provides specific guidelines for safeguarding ePHI, addressing various storage media and transmission methods. Examples include data stored on personal computers, external drives, magnetic tapes, USB devices, smartphones, or transmitted via email or network connections.
When it comes to cloud storage solutions, HIPAA considers such providers as Business Associates (BAs). These companies must sign Business Associate Agreements (BAAs) with covered entities, clarifying liability and security responsibilities. A well-drafted BAA includes provisions that specify safeguards, breach notification procedures, and compliance obligations to protect the confidentiality of stored health data. For detailed guidance on implementing robust safeguards, organizations can consult this implementation guide on effective AI use in healthcare.
How Can Organizations Achieve Compliance?
Navigating HIPAA’s Privacy and Security Rules can be complex, requiring extensive documentation, training, and ongoing monitoring. Managing PHI involves regular risk assessments, policy development, and staff education to ensure adherence to legal standards.
Organizations like Compliancy Group offer solutions that simplify compliance management. Their platform, The Guard, automates much of the process, providing real-time updates, policy management, and training modules. This approach helps organizations stay current with evolving regulations without incurring additional costs as rules expand or change. To learn more about safeguarding health data, visit the resource explaining electronic data interchange (EDI) in healthcare.
By implementing these measures, healthcare organizations can better protect patient data, reduce risk, and ensure regulatory compliance, ultimately fostering trust and integrity within the healthcare system.





