Understanding Healthcare Revenue Cycle Management and Its Impact on Patient Care
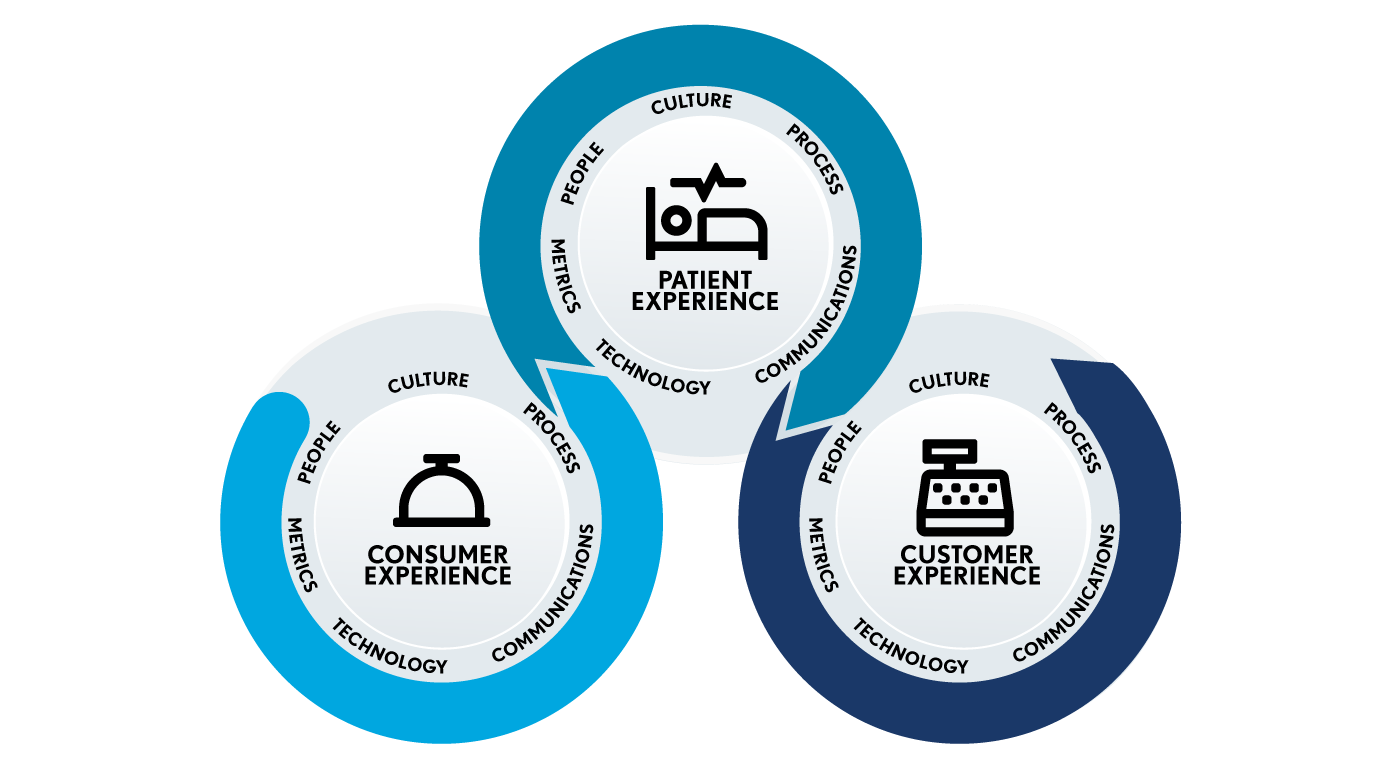
Healthcare revenue cycle management (RCM) is a vital process that healthcare providers rely on to ensure financial stability while delivering quality patient care. It encompasses all activities involved in capturing revenue from the moment a patient interacts with the healthcare system until the final payment is received. This comprehensive approach includes scheduling appointments, verifying insurance, delivering care, submitting claims, and managing reimbursements. Effective RCM is essential not only for maintaining the financial health of healthcare organizations but also for enhancing the patient experience by streamlining administrative processes and fostering transparency.
The success of revenue cycle management hinges on meticulous coordination among various components. These include patient registration, insurance verification, clinical documentation, claims processing, and accounts receivable management. Each step must be executed with precision to avoid delays and denials that can impede cash flow and patient satisfaction. Healthcare organizations increasingly recognize that fostering clear communication, promoting price transparency, and supporting equitable access to care are crucial elements. For example, providing patients with detailed cost estimates and helping them navigate financial assistance options can significantly improve their engagement and trust.
One of the key aspects of revenue cycle management involves financial conversations with patients. Educating patients about their insurance coverage, potential costs, and payment responsibilities helps set realistic expectations and encourages timely payments. HFMA has published best practices to guide these discussions, emphasizing when and where financial talks should take place, who should participate, and what topics to cover. These conversations not only foster transparency but also contribute to a positive healthcare experience.
Accurate documentation of care received is fundamental to the claim submission process. Charge capture ensures that every service provided is properly documented, which is critical for insurance reimbursement. Mistakes or omissions in documentation can lead to claim denials, delays, and revenue loss. Healthcare claim processing is a specialized area requiring attention to detail and data integrity. Timely, complete, and correct claims are essential to avoid denials and ensure prompt reimbursement. When claims are denied, healthcare providers must engage in appeals and denial management processes, which demand expertise and persistence.
Effective medical account resolution is another vital component of the revenue cycle. It involves engaging patients to settle their bills respectfully and efficiently, offering financial assistance or flexible payment plans when appropriate. Skilled account resolution specialists work to resolve outstanding balances while maintaining a positive patient relationship. This approach helps healthcare organizations reduce bad debt and improve overall revenue cycle performance, aligning with industry standards and best practices outlined by HFMA. For more insights, see HFMA’s Best Practices for Medical Account Resolution.
Interesting:
Throughout every phase, the patient experience remains a priority. The healthcare revenue cycle is often a patient’s first and last impression of the organization, influencing their overall perception and likelihood of returning for future care. By focusing on transparency, effective communication, and respectful engagement, healthcare providers can build trust and foster loyalty.
To stay current with industry advancements, many organizations pursue continuous education and certification. Resources such as HFMA’s e-learning courses and webinars help professionals stay ahead of trends and improve their skills. Additionally, programs like the Certified Revenue Cycle Representative (CRCR) credential validate expertise and enhance career prospects. Recognizing excellence in revenue cycle management, HFMA’s MAP Keys and MAP Award highlight organizations that meet or exceed industry benchmarks and demonstrate outstanding patient satisfaction.
Events like the HFMA Revenue Cycle Conference gather industry leaders to share strategies for improving financial performance and patient care. The Revenue Cycle Forum provides a collaborative space for professionals to explore common challenges and develop innovative solutions. Job boards and career resources further support professionals seeking growth opportunities in healthcare finance.
Organizations looking to optimize their revenue cycle operations can also explore trusted solutions recognized by HFMA’s Peer Review program. These vetted products and services span critical areas such as billing compliance, coding, denial management, patient access, and revenue cycle outsourcing. Implementing proven tools and practices can lead to more efficient workflows, increased revenue, and improved patient experiences.
For further information, explore virtual reality in medicine perspectives and features to see how emerging technologies are transforming healthcare delivery, training, and patient engagement. Similarly, innovative approaches like immersive therapy are opening new avenues for mental health treatment, as discussed in this insightful resource. Virtual reality also plays a significant role in training surgeons of tomorrow, offering realistic simulations that enhance surgical skills, which you can learn more about at this site. Furthermore, the intersection of sports and virtual reality is revolutionizing athletic training and performance, as highlighted here.





