Extracorporeal Membrane Oxygenation, commonly known as ECMO, is a sophisticated form of life support designed for patients experiencing severe heart or lung failure. This advanced medical procedure functions outside the body, providing critical assistance when traditional treatments are insufficient. ECMO has revolutionized intensive care by offering a temporary but vital bridge to recovery, supporting patients during their most fragile moments. Its use has expanded significantly over recent decades, especially in cases involving respiratory infections, heart attacks, or traumatic injuries. For those interested in how healthcare systems assess patient needs and allocate resources, exploring topics like the case mix index can offer valuable insights into hospital performance and patient outcomes.
ECMO involves a complex process where blood is diverted from the body, oxygenated externally, and returned seamlessly, mimicking the natural functions of the lungs and heart. This procedure can be life-saving, giving the organs time to heal or rest while the underlying condition is treated. Whether used as a bridge to transplantation or recovery, ECMO is reserved for critically ill patients who do not respond to conventional therapies. Its application requires highly specialized teams and equipment, making it available in only a select number of hospitals worldwide. According to the Extracorporeal Life Support Organization, over 21,000 ECMO procedures were performed globally in 2024, highlighting its vital role in modern critical care.
What Is ECMO and How Does It Work?
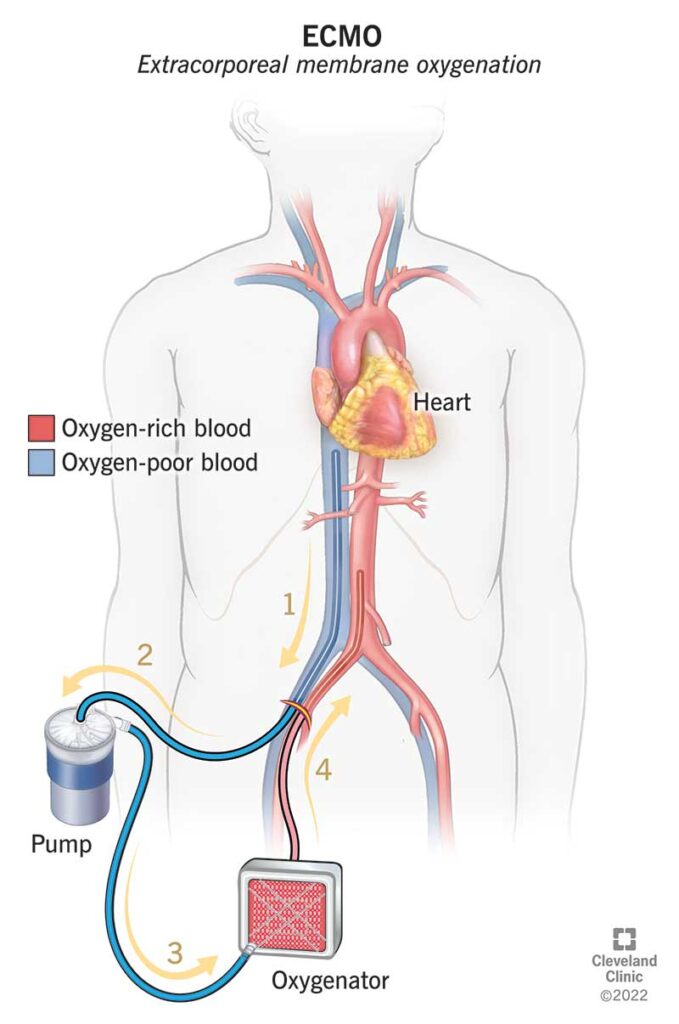
ECMO stands for extracorporeal membrane oxygenation—a term that reflects its core function. “Extracorporeal” means outside the body, indicating that blood is temporarily rerouted through a machine. This machine adds oxygen to the blood and removes carbon dioxide, essentially performing the gas exchange functions normally carried out by healthy lungs. The process involves inserting tubes, known as cannulas, into large blood vessels in the chest, neck, or legs. These tubes allow blood to flow out of the body, be processed in the ECMO device, and then return to circulation. During this time, patients are usually sedated, although some may remain awake, depending on their condition.
Healthcare providers continuously monitor heart and lung functions throughout ECMO therapy. Regular assessments help ensure the machine functions correctly and that no complications arise. When the patient’s condition improves, medical teams gradually reduce ECMO support in a process called weaning, which typically lasts from two to five days. Once stable, the tubes are removed, and the insertion sites are stitched up. The duration of ECMO support varies widely—from a few hours to several weeks—based on the underlying illness and response to treatment. This flexibility allows healthcare providers to tailor interventions to each patient’s needs, providing critical time for recovery.
Conditions Treated with ECMO
ECMO is primarily used for patients experiencing life-threatening respiratory or cardiac failure. It can support individuals suffering from severe pneumonia, acute respiratory distress syndrome, or heart failure. The procedure can also serve as a bridge to transplantation by maintaining organ function during the wait for a donor heart or lungs. In recent years, ECMO has gained prominence in managing complications from COVID-19, especially for patients who do not respond to mechanical ventilation. Its ability to perform gas exchange outside the body makes it invaluable in these critical scenarios.
In addition to its role in respiratory support, ECMO can help patients recover from trauma or cardiac events, such as heart attacks or severe infections. It provides a window of opportunity for treatments that might not otherwise be possible. Healthcare providers often use ECMO in conjunction with other therapies, including medications and interventions aimed at addressing the root cause of illness. The decision to initiate ECMO depends on various factors, including the severity of illness, the patient’s overall health, and available resources.
Interesting:
Risks and Complications of ECMO
While ECMO can be lifesaving, it also carries significant risks. Potential complications include bleeding, due to the necessity of blood-thinning medications to prevent clot formation in the circuit. Blood clots can cause strokes or other issues if not carefully managed. Kidney failure is another concern, especially if blood flow to the kidneys diminishes during treatment. In such cases, dialysis may be required temporarily or permanently. Additionally, the insertion of large cannulas can lead to tissue damage, particularly in the legs, which may necessitate surgical intervention or even amputation in rare instances.
Other risks include infections, since the procedure involves invasive tubes and devices breaching the skin barrier. Close monitoring and strict infection control measures are essential to minimize this danger. Because of these potential complications, ECMO is typically reserved for patients with the highest chance of benefit, and every effort is made to weigh the risks against the potential for recovery. Understanding these dangers underscores the importance of experienced healthcare teams and comprehensive patient management.
Who Benefits from ECMO?
The success of ECMO varies depending on the underlying condition, patient age, and overall health. Neonates and infants with respiratory failure often have high survival rates—ranging from 40% to 80%. For adults, survival rates tend to be lower, with about 30% to 50% living beyond five years after treatment. Advances in technology and clinical protocols continue to improve outcomes, making ECMO an increasingly vital option for critically ill patients. However, it is not suitable for everyone. Conditions such as irreversible brain injury, severe bleeding disorders, or certain contraindications may preclude its use. Healthcare providers evaluate each case carefully to determine if ECMO is appropriate.
The decision to proceed with ECMO involves multidisciplinary teams, including intensivists, cardiothoracic surgeons, and specialized nurses. They consider various factors, including the likelihood of recovery, potential quality of life post-treatment, and resource availability. As with any complex medical intervention, informed consent and family discussions are integral parts of the process. For more insights into how hospitals assess patient needs, exploring topics like the case mix index can shed light on healthcare resource allocation and patient outcomes, especially in critical care settings.
Conclusion
ECMO represents a remarkable advancement in critical care medicine, offering hope to patients with life-threatening heart and lung conditions. Despite its complexities and risks, when used appropriately, it can serve as a vital bridge to recovery or transplantation. As research continues and technology improves, ECMO’s role in saving lives is expected to expand further. If you or a loved one face such critical health challenges, discussing options with healthcare professionals can clarify whether ECMO might be a suitable intervention. Modern medicine’s understanding of how best to utilize this technology is ever-growing, helping clinicians make informed decisions that could ultimately save lives.
For more information on how healthcare systems evaluate and optimize patient care, consider reviewing resources like the impact of the case mix index and the significance of the case mix index. Additionally, when considering treatments like CBD in health settings, understanding key considerations can be vital—more on this can be found in navigating the use of CBD in healthcare settings key considerations.