Transforming Healthcare Through Artificial Intelligence in Clinical Practice
The rapid advancements in artificial intelligence (AI) are reshaping the landscape of healthcare, offering innovative solutions to longstanding challenges in clinical practice. As healthcare systems become increasingly complex, integrating AI technologies holds the promise of enhancing diagnostic accuracy, streamlining workflows, and personalizing patient care. To harness these benefits responsibly, it is essential to understand AI’s current capabilities, limitations, and future potential within medical settings. This exploration aims to provide a comprehensive overview of AI’s transformative role in healthcare, emphasizing its applications, ethical considerations, and strategies for effective implementation.
Introduction
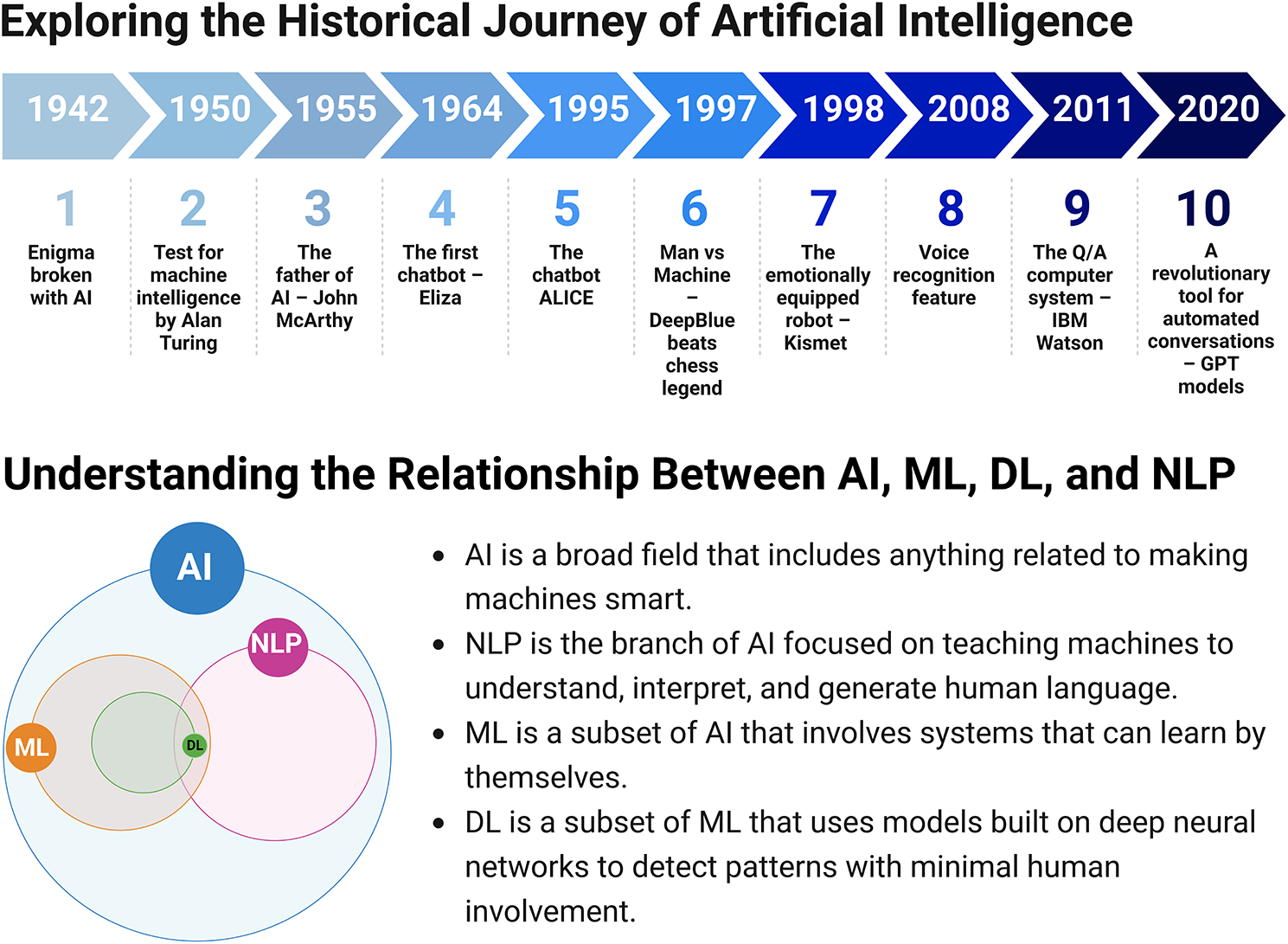
Artificial intelligence embodies the pursuit of creating machines capable of performing tasks traditionally requiring human intelligence. This encompasses diverse techniques such as machine learning (ML), deep learning (DL), natural language processing (NLP), and large language models (LLMs). These technologies enable systems to analyze vast datasets, interpret complex patterns, and generate insights that support clinical decisions. For instance, NLP allows computers to comprehend and produce human language, facilitating applications like medical record summarization or virtual health assistants. Over decades, AI has evolved from rule-based systems to sophisticated algorithms capable of learning and adapting, profoundly influencing sectors like finance, transportation, and notably, medicine.
Historically, AI’s journey began in the 1950s with pioneering programs, culminating in the 1956 Dartmouth Conference that officially coined the term “Artificial Intelligence.” Subsequent decades saw shifts from rule-based expert systems to neural networks and ML algorithms, with milestones such as IBM’s Deep Blue defeating chess grandmasters and virtual assistants like Siri and Alexa revolutionizing user interactions. Today, AI’s impact is most palpable in healthcare, where it aids in diagnostics, treatment planning, and patient monitoring. For example, AI tools analyzing medical images can detect cancers earlier than traditional methods, thus improving survival rates. As reported in making a difference how ai is helping the healthcare sector, AI’s integration into clinical workflows is essential for delivering high-quality, efficient care.
The rapid progress of AI technologies presents an unprecedented opportunity to revolutionize clinical practice. Documenting and disseminating insights into AI’s roles and limitations is vital for healthcare providers to adopt these tools effectively. This review explores the current state of AI in medicine, its applications across diagnostics, therapeutics, and population health management, and discusses the ethical and practical considerations necessary for responsible implementation.
Materials and Methods
An extensive review of relevant literature was conducted using key databases such as PubMed/Medline, Scopus, and EMBASE. The search was unrestricted by publication date but limited to articles written in English. Keywords included combinations related to AI applications in healthcare: NLP in healthcare, ML in medicine, DL in diagnostics, and AI-driven personalized medicine. The selection process involved screening titles and abstracts to identify studies that evaluate AI’s impact on clinical workflows, diagnostics, and treatment outcomes. Disagreements among reviewers were resolved through discussion, ensuring a comprehensive and balanced analysis.
AI Assistance in Diagnostics
Improving Diagnostic Accuracy
Disease diagnosis remains a critical challenge, complicated by the complexity of disease mechanisms and symptom overlap. AI, especially ML, leverages large datasets to identify subtle patterns beyond human perceptibility, thereby enhancing diagnostic precision. Deep learning models, utilizing convolutional neural networks (CNNs), excel in image analysis—detecting lesions in radiographs, MRIs, or pathology slides with remarkable sensitivity and specificity. For instance, AI systems trained on mammogram datasets have demonstrated a reduction in false positives and negatives, significantly improving breast cancer detection rates. A UK-based study showed that AI interpretation of mammograms reduced false positives by 5.7% and false negatives by 9.4%, illustrating its potential to augment radiologists’ capabilities see a brief history when was ai first used in healthcare.
Similarly, AI systems outperform clinicians in detecting skin cancers, such as melanoma, by analyzing dermoscopic images with accuracy comparable to expert dermatologists. In cardiovascular medicine, AI algorithms accurately predict risk factors from EKG data and imaging, enabling earlier interventions. Notably, AI models diagnosing pneumonia from chest X-rays have achieved sensitivities of 96%, surpassing traditional radiologist assessments. These advances demonstrate AI’s capacity to improve diagnostic accuracy, reduce costs, and accelerate decision-making, which is crucial in emergency settings. Incorporating AI into diagnostics can also minimize human errors and support clinicians with real-time insights, ultimately elevating patient outcomes.
Enhancing Laboratory Testing
Clinical laboratory testing provides foundational data for disease identification and management. AI’s integration into laboratory workflows improves the speed and precision of microbiological diagnostics. ML models analyze genomic sequences, microscopic images, and biochemical data to identify pathogens, determine antibiotic susceptibility, and predict disease progression. For example, AI systems analyzing microscopic images of blood samples can classify microorganisms with high sensitivity and specificity, expediting diagnosis and appropriate therapy see diagnostic testing for people with appendicitis using machine learning techniques.
Moreover, AI accelerates the detection of infectious agents such as malaria or tuberculosis by analyzing imaging or molecular data rapidly and cost-effectively. Automated identification of microorganisms enhances laboratory throughput, reduces manual errors, and informs timely treatment decisions. As a result, AI-driven laboratory diagnostics offer improved efficacy and efficiency, leading to faster results within 24–48 hours, which is critical for infectious disease management and controlling outbreaks.
AI Assistance in Treatment
Personalized Medicine and Decision Support
Personalized or precision medicine tailors treatments based on individual genetic, environmental, and lifestyle factors. AI enhances this process by analyzing complex datasets to predict treatment responses and optimize therapeutic strategies. For example, AI models trained on gene expression profiles can forecast chemotherapy efficacy in cancer patients, enabling clinicians to select the most effective regimens and avoid unnecessary toxicity see AI assistance in diagnostics.
Support systems powered by AI analyze electronic health records (EHRs) to predict responses to antidepressants or chemotherapeutic agents, reducing trial-and-error prescribing. These tools improve treatment outcomes, increase patient safety, and reduce healthcare costs. For instance, AI algorithms predicting treatment response in oncology have achieved over 80% accuracy, guiding clinicians toward more effective interventions. Further, AI-driven dose optimization platforms like CURATE.AI dynamically adjust chemotherapy doses based on real-time patient responses, improving efficacy and minimizing adverse effects see future outlook how ai can be used to solve medical challenges.
Interesting:
- How artificial intelligence is transforming cost reduction in healthcare
- Transforming healthcare through artificial intelligence four key examples of innovation
- Unlocking the potential of artificial intelligence in healthcare policy and practice
- Transforming healthcare through artificial intelligence
Dose Optimization and Therapeutic Monitoring
AI’s role extends to dose calculation and monitoring of drugs with narrow therapeutic indices, such as warfarin or immunosuppressants. Machine learning models analyze patient-specific data—including genetics, lab results, and medication history—to recommend personalized dosing regimens, reducing adverse events and improving efficacy. For example, AI systems predicting warfarin doses have outperformed clinicians, leading to more stable anticoagulation levels. AI also supports therapeutic drug monitoring (TDM), forecasting drug interactions and adverse reactions before they occur, thus safeguarding patient safety see AI assistance in population health management.
AI in Population Health Management
Predictive Analytics and Risk Stratification
Population health management benefits from AI-driven predictive analytics that identify at-risk groups for chronic diseases, hospital readmissions, and outbreaks. Machine learning models analyze demographic, clinical, and social determinants of health to forecast disease onset and progression, enabling targeted interventions. For example, predictive models can flag patients at high risk for diabetes or cardiovascular diseases, allowing early preventative measures. Similarly, hospital readmission risk models help allocate resources effectively and reduce healthcare costs.
AI also optimizes vaccine distribution and supply chain logistics, ensuring timely availability where most needed. In Saudi Arabia, analysis of social media health data identified prevalent diseases, demonstrating AI’s capacity to inform public health strategies see AI in population health management.
Developing Guidelines and Frameworks
AI facilitates the rapid synthesis of emerging research data, supporting the development of evidence-based clinical guidelines. Automated analysis of trial results and real-world evidence accelerates updates to protocols, ensuring clinicians have access to the latest recommendations. Several organizations are working on frameworks for AI validation, transparency, and ethical use, including the US FDA’s guidelines for AI/ML-based medical devices and the European Commission’s AI strategy. These efforts aim to ensure AI applications are safe, fair, and accountable, fostering trust among clinicians and patients alike see establishing guidelines for AI.
AI Assistance in Drug Information and Patient Care
Enhancing Drug Accessibility and Safety
AI-powered virtual assistants and chatbots are transforming how patients access medication information and medical advice. These tools provide real-time, evidence-based responses, remind patients about medication adherence, and answer common health questions, reducing the burden on healthcare providers. For example, AI chatbots used in NHS settings handle millions of queries efficiently, improving accessibility and patient engagement see AI virtual healthcare assistance.
Mental Health Support
AI applications are increasingly employed in mental health care, offering personalized support through internet-based cognitive behavioral therapy (CBT) and symptom monitoring. Digital mental health tools can detect early signs of depression or anxiety, providing round-the-clock support and reducing barriers to care. Although promising, these applications must be carefully designed to mitigate biases and ensure empathy remains central to mental health treatment. Studies show that AI tools like Woebot can improve symptoms of substance use disorder and depression, highlighting their potential as adjuncts to traditional therapy see AI in mental health support.
Improving Patient Education and Reducing Provider Burnout
AI-driven chatbots customize educational content, helping patients understand their diagnoses and treatment plans at appropriate literacy levels. For example, chatbot tools have increased patient knowledge about prostate cancer and diabetes management. These resources empower patients, foster adherence, and reduce anxiety. Additionally, AI can reduce healthcare provider burnout by automating routine tasks and supporting clinical decision-making, allowing clinicians to focus on complex cases and compassionate care see improving patient care.
Future Directions and Challenges
Overcoming Barriers to Implementation
Despite promising developments, integrating AI into clinical workflows faces obstacles such as data privacy concerns, limited high-quality datasets, and algorithm bias. Ensuring data security and patient confidentiality is paramount, necessitating strict adherence to regulations like HIPAA and GDPR. Additionally, AI models must be transparent, explainable, and validated across diverse populations to prevent biases that could compromise care quality. Developing multidisciplinary collaborations between clinicians, data scientists, and ethicists is vital to create robust, trustworthy AI tools.
Training healthcare professionals in AI literacy is equally important. Incorporating AI education into medical curricula ensures future clinicians can effectively evaluate and utilize these technologies. Moreover, regulatory frameworks need to evolve to assess AI tools’ safety and efficacy, with agencies like the FDA and EMA leading these efforts. Ethical considerations, including accountability, transparency, and equity, must underpin AI deployment to foster trust and acceptance.
Ethical, Legal, and Social Implications
AI’s adoption raises questions around accountability in case of errors, potential biases, and impacts on the patient-provider relationship. Maintaining human oversight in AI-assisted decision-making is essential to ensure ethical standards are upheld. Legal frameworks should clarify liability issues, and continuous monitoring must detect and mitigate unintended consequences. As AI becomes more embedded in healthcare, a balanced approach that combines technological innovation with human compassion remains crucial.
Conclusion
Artificial intelligence has the transformative potential to revolutionize clinical practice, improving diagnostic accuracy, personalizing treatments, and enhancing population health management. Its integration can lead to more efficient, equitable, and effective healthcare systems. However, realizing this promise requires addressing technical, ethical, and regulatory challenges through collaborative efforts among stakeholders. Investing in education, robust data security, and transparent validation processes will pave the way for AI to serve as a trusted partner in medicine, ultimately elevating patient care and health outcomes worldwide. For further insights on how AI is shaping various aspects of medicine, visit a future outlook on AI’s role in solving medical challenges, and explore detailed applications in patient care at improving patient outcomes.





