Navigating the Role of Clinical Decision Support Systems in Modern Healthcare
The integration of clinical decision support systems (CDSS) has revolutionized healthcare delivery by providing clinicians with advanced tools to enhance decision-making, improve patient safety, and streamline workflows. As these systems become more sophisticated and widespread, understanding their benefits, potential pitfalls, and strategies for effective implementation is crucial for healthcare providers, administrators, and policymakers alike. This comprehensive overview explores the various types of CDSS, their current applications, advantages, inherent challenges, and best practices to maximize their positive impact while minimizing risks.
Abstract
Computerized clinical decision support systems are transforming healthcare practices by assisting clinicians in complex diagnostic and therapeutic decisions. Since their inception in the 1980s, these systems have evolved rapidly, now often embedded within electronic medical records and integrated clinical workflows, driven by the global adoption of advanced electronic health records (EHRs). Despite their promising potential, uncertainties remain regarding their influence on healthcare providers, patient outcomes, and associated costs. Past successes have been noted, but notable setbacks highlight the risks involved. This article offers a detailed, current overview of CDSS in medicine, covering different system types, effective use cases, common pitfalls, and possible harms. It concludes with evidence-based recommendations for designing, implementing, and maintaining CDSS to ensure safety and efficacy.
Introduction: What is a clinical decision support system?
A clinical decision support system (CDSS) is designed to enhance healthcare quality by providing healthcare professionals with tailored clinical knowledge, patient-specific data, and guidance at the point of care. Traditionally, these systems are software tools that assist clinicians by matching individual patient information against a comprehensive knowledge base, generating recommendations or assessments that inform clinical decisions. Over time, CDSS have expanded beyond simple rule-based alerts to leverage artificial intelligence (AI), machine learning (ML), and large datasets to uncover insights previously inaccessible to humans.
The origins of computer-based CDSS date back to the 1970s, although early iterations faced limitations such as poor system integration, high resource demands, and ethical dilemmas related to physician autonomy and accountability. Modern systems are typically integrated with electronic health records (EHR) and computerized provider order entry (CPOE) platforms, operating across multiple devices including desktops, tablets, smartphones, and wearable health monitors. This allows for real-time decision support at the bedside or in outpatient settings.
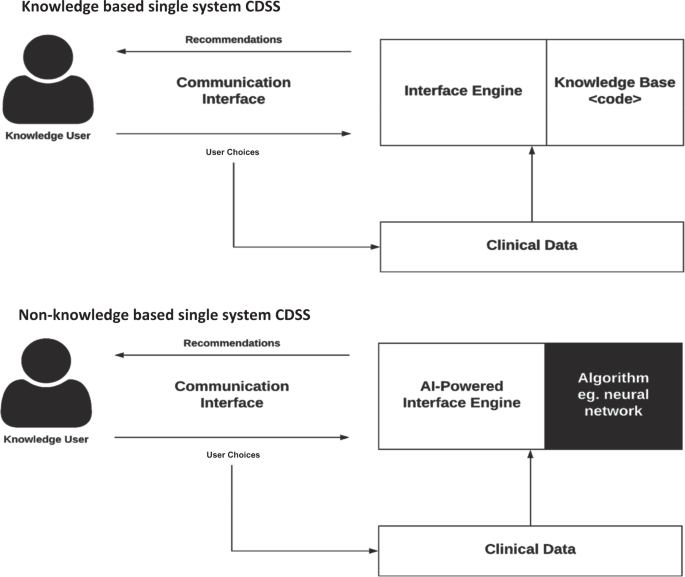
CDSS are categorized based on their operational features and delivery methods. They are generally divided into knowledge-based systems, which encode clinical rules derived from literature and practice guidelines, and non-knowledge-based systems that utilize AI and data-driven approaches like machine learning. These approaches differ in their transparency, complexity, and implementation challenges, with AI-based systems facing issues such as “black box” decision-making processes and data availability concerns.
Fig. 1: Diagram of key interactions in knowledge-based and non-knowledge-based CDSS.
They consist of core components: the knowledge base or algorithm, the inference engine that applies rules to patient data, and the communication interface through which clinicians interact with the system. The US government, recognizing their importance, has incentivized CDSS deployment through policies and financial support, leading to widespread adoption in hospitals across North America and Europe. For instance, in the US, approximately 40% of hospitals with EHRs have integrated some form of decision support, with many countries investing heavily in national health record initiatives.
These systems serve a broad array of functions, including diagnostic assistance, alerts for medication safety, disease management guidance, prescription support, and clinical workflow management. As this field advances, ongoing research continues to evaluate their effectiveness, safety, and integration strategies—aimed at harnessing their full potential while avoiding unintended consequences.
Box 1. Methods and sources used for this overview
- MEDLINE search 1980-January 2018, using keywords related to CDSS and clinical decision support
- Review of references and bibliographies from retrieved articles
- Academic texts and reports on healthcare technology and decision support
- Personal and institutional experience with health informatics systems
Functions and advantages of CDSS
Patient safety
Enhancing medication safety remains a core strength of CDSS. Systems designed to detect drug-drug interactions (DDIs) are among the most widely implemented safety features, as up to 65% of hospitalized patients may be exposed to potentially harmful drug combinations. Modern computerized provider order entry (CPOE) systems are equipped with safeguards that alert clinicians to dosing errors, duplicate therapies, and contraindications. While these alerts are vital, their implementation varies significantly across institutions, with differences in how alerts are prioritized, displayed, and integrated into workflows. Variability in alert relevance and timing can lead to “alert fatigue,” where clinicians become desensitized to warnings, potentially undermining safety.
Efforts like the US Office of the National Coordinator for Health IT have developed prioritized lists of high-risk DDIs to standardize alerts across systems. Complementary safety tools include electronic medication dispensing systems and barcode-assisted administration, which create a “closed-loop” medication process—covering prescribing, transcribing, dispensing, and administration—thus drastically reducing errors at the bedside. Despite high costs, studies have demonstrated significant reductions in medication errors with these technologies.
CDSS also support safety beyond medication management. For example, clinical alerts can prompt timely blood glucose measurements in ICU settings, decreasing hypoglycemia incidents. Overall, patient safety remains a primary objective, with CDSS reducing prescribing errors, contraindication oversights, and adverse drug events, thus contributing to safer healthcare environments.
Clinical management
CDSS are instrumental in promoting adherence to evidence-based guidelines. Traditional guideline implementation often suffers from low compliance, as clinicians find it challenging to stay updated or apply complex protocols consistently. By encoding guidelines into decision support tools—such as standardized order sets, reminders, and alerts—CDSS facilitate guideline-concordant care at the point of practice.
These systems assist in managing various aspects of clinical care, including patient tracking, follow-up scheduling, and protocol adherence. For instance, alerts can notify clinicians when patients are due for screenings or are eligible for clinical trials, streamlining research recruitment. An example includes a CDSS at Cleveland Clinic that prompts physicians to evaluate patient eligibility for ongoing clinical studies, thereby improving trial enrollment efficiency.
Cost containment
Implementing CDSS can lead to significant cost savings by optimizing resource utilization, reducing unnecessary tests, and suggesting more affordable medication alternatives. For example, a rule limiting laboratory testing to once every 24 hours in a pediatric ICU resulted in substantial savings without compromising patient outcomes. Similarly, drug substitution algorithms have enabled hospitals to automatically switch to formulary-preferred medications, reducing costs and minimizing errors.
In Germany, a hospital developed an automated drug-switch system integrated with CPOE, which correctly and safely switched a majority of medication consultations, demonstrating potential for reducing medication costs and improving safety. Such systems also alert providers to lower-cost options, contributing further to healthcare sustainability.
Administrative functions
CDSS support administrative tasks like accurate coding, procedure ordering, and patient triage. For example, visual tools linked to ICD codes can help emergency physicians assign accurate diagnoses quickly. Additionally, decision support enhances documentation quality, which is vital for clinical, billing, and legal purposes. An obstetric CDSS improved documentation of labor interventions, while another system increased the accuracy of vaccination alerts post-splenectomy, preventing secondary infections.
Diagnostics support
Diagnostic decision support systems (DDSS) assist clinicians in formulating accurate diagnoses. Early systems relied on rule-based algorithms, but recent developments incorporate machine learning techniques, increasing diagnostic precision. For example, systems designed to diagnose peripheral neuropathy or suggest possible diagnoses based on clinical features have achieved high accuracy, sometimes rivaling expert clinicians.
Interesting:
In imaging, knowledge-based CDSS can recommend appropriate tests, reduce unnecessary procedures, and flag contraindications. Advanced AI-driven tools analyze vast amounts of imaging data, enabling early tumor detection and disease classification, often matching or exceeding human expert performance. Similarly, CDSS for laboratory and pathology interpretation assist in tumor grading, blood analysis, and genetic testing, supporting a wide range of diagnostic activities.
Patient-facing decision support
The emergence of Personal Health Records (PHRs) integrated with CDSS provides patients with tools to participate actively in their care. Such systems facilitate shared decision-making by providing tailored information, symptom tracking, and interactive features. For example, wearable glucose monitors connected to PHRs enable continuous monitoring and communication between patients and providers, improving disease management and engagement.
Systems like Vanderbilt’s MyHealthAtVanderbilt exemplify how integrated PHRs can deliver personalized educational content, track symptoms, and support self-management. As these platforms evolve, their focus is shifting toward fostering patient involvement, making care more participatory and aligned with individual preferences.
Pitfalls of CDSS
Fragmented workflows
Poorly designed or standalone CDSS can disrupt clinical workflows, leading to inefficiencies and clinician frustration. Early systems often required extra documentation or manual data entry, adding cognitive burden. Even well-integrated systems may create disconnects between face-to-face interactions and digital prompts, reducing their utility. Experienced clinicians may override or ignore alerts, especially if they perceive them as irrelevant, highlighting the importance of designing systems with user input and workflow considerations.
Alert fatigue and inappropriate alerts
High volumes of non-specific or low-value alerts cause clinicians to develop alert fatigue, resulting in ignored or dismissed warnings. Studies report that up to 95% of alerts may be inconsequential. Critical alerts should be prioritized to avoid desensitization, but even life-saving alerts can be misaligned with clinical context, leading to false positives or unnecessary interruptions. Customizing alert thresholds and relevance is essential to maintaining clinician trust and system effectiveness.
Impact on user skill
Over-reliance on CDSS may diminish clinicians’ diagnostic and procedural skills over time. The “carry-over” effect suggests that system use can reduce the need for independent judgment, potentially eroding expertise. Conversely, excessive trust in these tools may lead to complacency or errors if the system fails or provides inaccurate recommendations. Balancing support with maintaining core competencies is crucial for sustainable clinical practice.
Dependence on computer literacy
Effective use of CDSS requires appropriate technological skills. Overly complex systems can hinder adoption, especially among users with limited digital literacy. Training and system design should account for varying levels of user proficiency, incorporating intuitive interfaces and optional guidance features like info buttons to facilitate understanding and reduce frustration.
System and content maintenance
Keeping CDSS up to date with current guidelines, evidence, and clinical practices is challenging yet vital. Outdated knowledge bases can lead to suboptimal or unsafe recommendations. Regular technical maintenance, content review, and updates are necessary but often overlooked, risking system obsolescence and reduced trust among clinicians.
Data quality and content accuracy
CDSS depend on accurate, complete, and current data. Poor data quality, such as outdated medication lists or incomplete patient information, compromises decision support accuracy. External factors like inventory shortages or system workarounds can further impair functionality. Standardized coding systems like SNOMED CT and ICD are essential for interoperability and reliable decision support.
Interoperability challenges
Despite progress, many CDSS lack seamless integration across different health IT systems. Stand-alone or incompatible platforms hinder data sharing, reducing system utility. Adoption of interoperability standards like HL7 and FHIR is improving connectivity, but widespread, uniform implementation remains a work in progress. Cloud-based solutions offer promising avenues for enhanced interoperability and data sharing, with appropriate security measures in place.
Financial challenges
Initial costs for deploying CDSS are significant, and ongoing expenses for updates, training, and maintenance can strain budgets. Evaluations of cost-effectiveness are varied and complex, influenced by local contexts and system maturity. Demonstrating tangible return on investment remains a challenge, but long-term benefits often include improved safety, efficiency, and patient outcomes.
Conclusion
Clinical decision support systems are vital tools that support and augment healthcare delivery across diverse settings. Their proven benefits in enhancing safety, promoting evidence-based care, and reducing costs are well documented, especially for systems integrated with order entry and documentation workflows. As technology advances—particularly with AI, improved interoperability, and patient engagement—the potential for CDSS to further transform medicine grows. However, careful attention must be paid to design, implementation, and ongoing maintenance to avoid pitfalls such as workflow disruption, alert fatigue, data quality issues, and over-reliance. Conscientious planning and continuous evaluation are necessary to harness CDSS as effective, safe, and sustainable components of modern healthcare.
References
- Osheroff, J. et al. Improving Outcomes with Clinical Decision Support: An Implementer’s Guide. (HIMSS Publishing, 2012).
- Sim, I. et al. Clinical decision support systems for the practice of evidence-based medicine. J. Am. Med. Inf. Assoc. 8, 527–534 (2001).
explaining electronic data interchange in healthcare
from molecules to market the new era of pharmaceutical visualization
everything you need to know about emr systems in healthcare
the advantage factor how is ai helpful in healthcare diagnosis





