Navigating RFI and RFP Processes in Healthcare Procurement
Understanding how healthcare organizations acquire goods and services is crucial for vendors and procurement teams alike. The processes of Request for Information (RFI) and Request for Proposal (RFP) are foundational tools that facilitate transparent, efficient, and compliant purchasing. As healthcare systems become more complex and regulated, mastering these processes ensures timely, accurate, and fair vendor evaluations—ultimately impacting patient care and operational efficiency.
Procurement in healthcare extends beyond administrative paperwork; it directly influences clinical outcomes, safety standards, and regulatory adherence. When hospitals or clinics select improper vendors or delay essential procurements, the consequences can ripple across safety, compliance, and financial performance. Therefore, structured and well-managed procurement processes are vital. Many organizations utilize RFIs and RFPs as part of their strategic approach, but understanding their distinct roles, timing, and best practices remains essential for optimizing results.
In this discussion, we clarify what constitutes an RFI and RFP in healthcare, highlight their key differences, and explore how to manage these tools effectively to reduce delays, improve proposal quality, and ensure compliance. We also address common challenges faced by healthcare procurement teams and vendors, and how emerging AI solutions are transforming this landscape, enabling faster and more accurate responses.
What Is an RFI in Healthcare Procurement?
An RFI serves as an initial step in the procurement journey, designed to gather broad, preliminary information about market options, vendor capabilities, and available technologies. It is a formal document that helps healthcare organizations explore potential solutions without committing to any specific vendor or solution at this stage.
Why Use an RFI?
The primary purpose of an RFI is to support comprehensive market research. Healthcare organizations utilize RFIs to understand the landscape, identify innovative solutions, and evaluate vendor qualifications. Typical scenarios include:
- Exploring advanced medical devices or diagnostic equipment
- Assessing healthcare IT solutions or software platforms
- Investigating telehealth services or facility management options
- Evaluating specialized clinical service providers
For instance, a hospital considering new imaging technology might issue an RFI to collect specifications, pricing estimates, and vendor experience. This approach enables decision-makers to formulate an informed strategy before issuing a formal RFP.
Structure of a Typical Healthcare RFI
A well-structured RFI usually includes:
- Introduction: An overview of the organization and project context.
- Information Requested: Specific questions about vendor capabilities, services, and solutions.
- Response Guidelines: Instructions for submission format and process.
- Timelines: Deadlines for responses and subsequent steps.
RFIs are deliberately broad and exploratory; they do not seek finalized proposals but instead inform the subsequent procurement stages.
Benefits of Using RFIs
Implementing RFIs offers several advantages:
- Time Efficiency: Quickly filters vendors who do not meet basic requirements.
- Transparency: Standardized questions promote fair and consistent data collection.
- Scope Clarification: Defines needs early, reducing scope creep during later stages.
What Is an RFP in Healthcare Procurement?
Once the initial market exploration is complete, healthcare organizations often issue an RFP to solicit detailed, competitive bids from qualified vendors. An RFP is a comprehensive, structured document that invites vendors to submit proposals tailored to the organization’s specifications.
Why Are RFPs Used?
An RFP enables healthcare providers to compare vendor responses based on technical, financial, and compliance criteria. It signals readiness to evaluate detailed solutions and select the most suitable partner. For vendors, understanding the RFP process is crucial for crafting compelling, compliant proposals.
Contents of a Healthcare RFP
Typically, an RFP includes:
- Background & Objectives: Context about the healthcare facility and project goals.
- Technical Requirements: Detailed specifications, integration needs, and performance standards.
- Compliance & Regulatory Standards: Requirements aligned with HIPAA, FDA, HITRUST, and local laws.
- Evaluation Criteria: Clear scoring metrics for proposals.
- Submission Process: Deadlines, contact points, and submission instructions.
For example, a hospital seeking a new electronic health record (EHR) system will specify technical and security requirements, along with compliance standards. Vendors respond with detailed proposals addressing each aspect, facilitating an objective comparison.
Common RFP Scenarios in Healthcare
Healthcare organizations issue RFPs for various needs, such as:
- EHR systems and health information platforms
- Diagnostic and imaging equipment
- Facility operations and management services
- Telehealth and patient engagement solutions
A typical case involves a hospital seeking a new EHR platform, issuing an RFP that details system integration, security measures, and compliance requirements. Vendors respond with comprehensive proposals aligned with these specifications.
Why RFPs Are Critical for Vendors
Responding effectively to RFPs can significantly influence vendor selection. A well-prepared proposal demonstrates accountability, aligns with client priorities, and enables fair comparison. Moreover, understanding what is RFP in healthcare helps vendors tailor their responses to meet precise needs and regulatory standards.
For more insights on healthcare systems, explore what is japans healthcare system.
Key Differences Between RFIs and RFPs in Healthcare
While RFIs and RFPs are interconnected components of procurement, they serve distinct purposes and occur at different stages. Recognizing these differences streamlines the procurement process and enhances vendor engagement.
Interesting:
- Navigating the healthcare system and insurance options in hong kong
- Navigating the challenges and opportunities of ai integration in healthcare
- Navigating the tension between market and social justice in healthcare
- Navigating healthcare in brazil a comprehensive guide for expats and residents
- Navigating and preventing conflicts of interest in healthcare
| Aspect | RFI | RFP |
| — | — | — |
| Purpose | Gather broad market information | Obtain detailed, competitive proposals |
| Stage | Early exploration and research | Final evaluation and selection |
| Level of Detail | High-level, general data | In-depth technical, financial, and compliance info |
| Response Formality | Informal, optional | Formal, binding submissions |
| Outcome | Vendor qualification, scope clarification | Contract award to the best-fit vendor |
Understanding these distinctions helps procurement teams deploy RFIs to refine requirements before issuing RFPs, ensuring responses are targeted and efficient.
Challenges in Traditional Healthcare RFI and RFP Processes
Despite their importance, traditional healthcare procurement processes face numerous hurdles:
1. Lengthy and Resource-Intensive Workflows
Manual document handling, extensive reviews, and approval cycles can extend procurement timelines, sometimes taking months or years. This delays critical procurements, impacting patient care and operational efficiency.
2. Fragmented Information and Silos
Departments such as clinical, IT, legal, and finance often operate independently, leading to inconsistent documentation and communication gaps. Vendors may struggle to provide comprehensive responses, risking disqualification.
3. Regulatory and Compliance Risks
Healthcare procurement requires strict adherence to regulations like HIPAA, FDA, and HITRUST. Overlooking or misrepresenting compliance details can lead to disqualification or legal penalties.
4. Lack of Standardized Templates
Inconsistent formats across departments complicate proposal evaluation and comparison, increasing the risk of errors and delays.
5. Poor Communication Tracking
Managing multiple vendor inquiries and responses through email or spreadsheets creates confusion, missed deadlines, and inefficient decision-making.
6. Human Errors in Evaluation
Manual scoring and review processes are susceptible to bias, oversight, and inconsistency, leading to potential selection of suboptimal vendors.
To address these challenges, healthcare organizations are increasingly turning to AI-powered solutions to streamline procurement workflows.
How AI Is Transforming Healthcare RFP and RFI Management
AI-driven tools revolutionize the traditional procurement landscape by automating repetitive tasks, enhancing accuracy, and accelerating decision-making. Features include:
- Automated Response Generation: Auto-populating proposals with vetted content, reducing time spent on routine questions.
- Enhanced Compliance Checks: Flagging missing or inconsistent documentation, ensuring regulatory adherence.
- Collaborative Platforms: Facilitating real-time review and feedback among cross-functional teams.
- Data Analytics: Providing insights into response performance, win rates, and process bottlenecks.
For instance, addressing the top clinical causes of insurance claim rejections becomes easier when AI tools help identify common compliance issues across proposals, reducing costly errors.
Ensuring Compliance in Healthcare RFPs
Regulatory compliance is paramount. Common pitfalls include incomplete documentation, vague security policies, and oversight of local laws. Here are essential considerations:
- Maintain an organized repository of HIPAA, FDA, and HITRUST documentation.
- Customize security protocols to match client-specific requirements.
- Incorporate awareness of state-specific healthcare laws, such as CCPA in California.
- Clearly define data retention, breach notification, and access policies, aligning with healthcare regulations.
Proactively addressing these aspects enhances bid credibility and reduces disqualification risks.
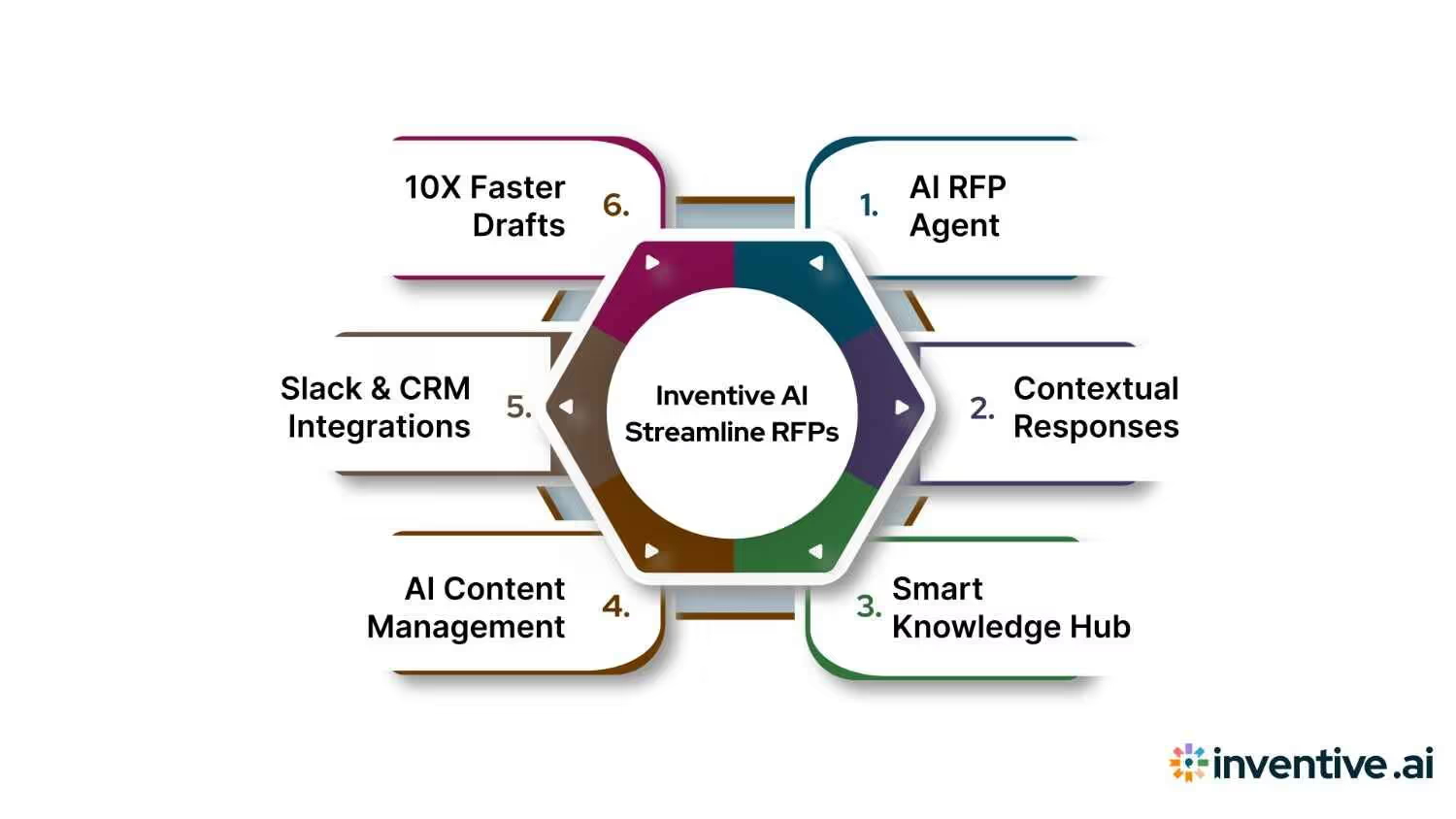
How Inventive AI Enhances RFP and RFI Processes
Inventive AI offers a suite of capabilities tailored for healthcare procurement:
- Automating proposal creation and scoring for faster, consistent responses.
- Generating compliant content aligned with HIPAA and other standards.
- Streamlining team collaboration through cloud-based review workflows.
- Providing analytics dashboards to monitor response quality and process efficiency.
By integrating AI, healthcare organizations and vendors can respond more swiftly, accurately, and confidently—reducing procurement cycle times and improving compliance.
Conclusion
Mastering the roles of RFIs and RFPs in healthcare procurement is essential for efficient, compliant, and strategic purchasing. While traditional processes are often slow and error-prone, AI-driven solutions are transforming how healthcare providers manage vendor selection and contract negotiations. Understanding these tools and leveraging technology ensures organizations can meet regulatory demands, reduce risks, and deliver better patient outcomes.
FAQs
1. How do RFIs and RFPs differ in healthcare procurement?
RFIs are preliminary inquiries used to explore market options and vendor capabilities, while RFPs are detailed requests for proposals focused on selecting a specific vendor based on comprehensive submissions.
2. Is pricing information included in RFIs?
Typically, RFIs do not focus on pricing; they gather high-level information. Pricing details are usually solicited during the RFP or RFQ stages when project scope is clearer.
3. When should a healthcare organization issue an RFQ instead of an RFP?
An RFQ is appropriate when project requirements are well-defined, and price is the primary consideration. RFPs are used for complex projects requiring detailed technical and compliance evaluations.
4. Why initiate with an RFI before issuing an RFP?
An RFI helps refine project needs, identify qualified vendors, and avoid broad or ineffective RFPs, leading to more targeted and efficient procurement.
5. How long does a typical healthcare RFP process take?
Procurement cycles can range from several months to over a year, depending on project complexity, regulatory review, and stakeholder involvement.
6. Do procurement teams review every RFI and RFP response thoroughly?
Yes, especially in regulated environments, responses are evaluated against structured criteria, emphasizing accuracy, compliance, and suitability.





