Navigating Ethical Challenges in Modern Healthcare
The constantly evolving landscape of healthcare presents numerous ethical dilemmas that professionals and patients alike must confront. In an environment where technological advancements, resource constraints, and societal values intersect, understanding these moral issues becomes essential for delivering compassionate, fair, and responsible care. This article explores some of the most pressing ethical questions faced today, illustrating how they influence decision-making processes, policy development, and everyday clinical practice. By examining real-world examples and foundational principles, we aim to shed light on the complexities of maintaining integrity and trust within healthcare systems.
Overview of Ethical Issues in Healthcare
Ethical challenges in healthcare encompass a broad spectrum of concerns affecting both patients and providers. At the core, issues such as obtaining informed consent are vital; ensuring patients fully understand their treatment options is fundamental to respecting their autonomy. Unfortunately, medical jargon and complex information can sometimes hinder genuine understanding, leading to decisions that may not reflect true patient preferences.
Equity in healthcare access remains a persistent concern. Socioeconomic disparities often determine the quality and availability of care received, creating systemic inequalities that undermine health outcomes for marginalized communities. For example, populations in underserved areas may lack access to specialized services, exacerbating health disparities.
End-of-life decision-making introduces profound moral questions. Balancing a patient’s right to choose their preferred course of care with family members’ wishes can be challenging. Respecting patient autonomy while navigating emotional family dynamics calls for sensitive communication and ethical clarity.
Resource allocation is another critical issue, particularly during crises like pandemics. When resources such as ICU beds or ventilators are scarce, determining who receives treatment involves difficult moral judgments—should age, prognosis, or social factors influence prioritization? These tough choices underscore the importance of transparent, ethically grounded policies.
Data privacy and information security are increasingly significant in digital health environments. Protecting sensitive personal health information from breaches, while maintaining transparency about data usage, is essential for maintaining trust. Healthcare providers must implement robust safeguards to ensure confidentiality and compliance with regulations like HIPAA.
Understanding these issues emphasizes the importance of ongoing ethical reflection and dialogue among stakeholders to improve health outcomes and uphold moral standards.
Key Ethical Principles
Guiding healthcare professionals through complex moral terrain are core principles rooted in bioethics, which help ensure fair and compassionate treatment.
Autonomy
Respect for patient autonomy involves honoring individuals’ rights to make informed decisions about their healthcare. For example, providing comprehensive information about treatment risks and benefits empowers patients to choose options aligned with their values. Ensuring clarity and transparency in communication fosters trust and respects personal agency.
Beneficence
The principle of beneficence obligates providers to act in the best interest of patients, promoting their well-being. Developing personalized treatment plans based on current evidence exemplifies this commitment. Beneficence encourages clinicians to weigh potential benefits against risks, aiming for interventions that improve health outcomes.
Non-maleficence
Non-maleficence, or “do no harm,” requires healthcare workers to avoid actions that could cause unnecessary suffering. For instance, prescribing medications after careful consideration of side effects safeguards patients from avoidable harm. This principle underscores the importance of diligent assessment and cautious intervention.
Justice
Justice emphasizes fairness in distributing healthcare resources and services. During emergencies, equitable allocation ensures that no group is unfairly disadvantaged. For example, prioritizing vulnerable populations during vaccine distribution reflects a commitment to social justice. Upholding justice fosters trust and legitimacy within healthcare systems.
Interesting:
- Navigating ethical challenges in modern healthcare
- Navigating ethical challenges in healthcare key issues shaping 2025
- Navigating ethical challenges in modern nursing practice
- Ethical frontiers addressing modern challenges in healthcare
- Understanding healthcare payers roles types and challenges in modern medicine
Major Ethical Issues in Healthcare
Addressing the most significant ethical concerns helps improve clinical practice and policy development.
Patient Privacy and Confidentiality
Maintaining confidentiality is fundamental to patient trust. Data breaches can lead to harm and erosion of confidence in healthcare providers. Implementing measures such as encryption, access controls, and staff training is crucial. For example, healthcare organizations must restrict access to sensitive information to authorized personnel and regularly update security protocols. Compliance with legal standards like HIPAA ensures accountability and protection.
Informed Consent
Ensuring patients are fully informed about their treatment options respects their right to choose. Without clear communication, patients may inadvertently consent to procedures they do not understand, risking adverse outcomes. Healthcare providers should use plain language, provide written materials, and encourage questions to facilitate comprehension. This transparency helps patients feel empowered and engaged in their care decisions.
Access to Care
Disparities in healthcare access continue to challenge equity. Rural residents or low-income populations often face obstacles such as distance, cost, or limited services. Strategies like expanding telemedicine, establishing community clinics, and policy reforms aim to bridge these gaps. Promoting universal access not only improves individual health but also enhances community resilience.
End-of-Life Decisions
Decisions regarding palliative care and life-sustaining treatments involve delicate moral considerations. Respecting advance directives and patient wishes is paramount, yet emotional and familial pressures can complicate choices. Facilitating open discussions, providing psychological support, and respecting autonomy help navigate these sensitive situations ethically.
Ethical Dilemmas Faced by Healthcare Professionals
Practitioners regularly confront conflicts that test their moral resolve and professional integrity.
Balancing Duty and Personal Beliefs
Healthcare workers may experience tension between their personal morals and professional responsibilities. For example, a nurse who opposes euthanasia on moral grounds may still be required to care for patients undergoing such procedures. Navigating these conflicts involves respecting personal convictions while adhering to ethical standards and institutional policies. Providing avenues for dialogue and support can assist staff in managing these dilemmas.
Resource Allocation
Limited resources demand difficult prioritization decisions. During a health crisis, determining which patients receive scarce interventions involves criteria such as prognosis and fairness. Transparency about decision-making processes enhances trust, though it can evoke emotional distress. Developing clear, ethically sound guidelines helps balance individual needs with collective good.
For further insights on maintaining ethical standards, healthcare institutions should explore protections for whistleblowers, who play a vital role in safeguarding integrity. Safeguarding ethical practices: the critical role of whistleblower protections in healthcare compliance emphasizes the importance of supporting personnel who report unethical behavior.
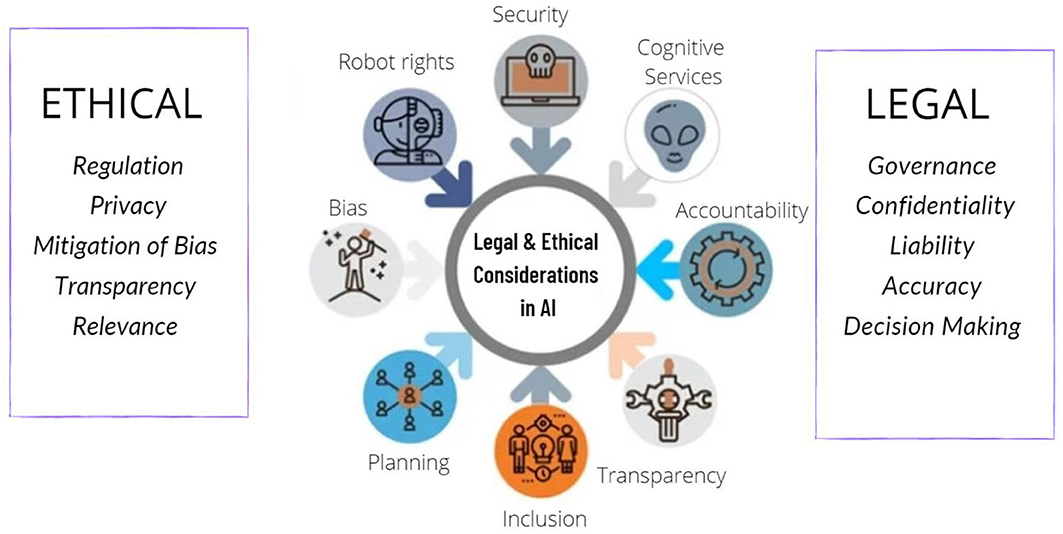
The rapid integration of artificial intelligence (AI) and digital tools in healthcare is transforming patient engagement and decision-making processes. For example, AI-driven solutions can enhance diagnostics and personalize treatments, but they also raise questions about accountability and transparency. To stay ahead, healthcare organizations need to embrace innovations while ensuring ethical standards are maintained. Learn more about how AI is shaping the future of patient care here.
Finally, addressing alert fatigue is critical for patient safety. Healthcare providers often face an overwhelming number of notifications from monitoring systems, which can lead to missed critical alerts or delayed responses. Effective strategies for navigating these challenges include optimizing alert systems and staff training to improve response accuracy. Read more about strategies for managing alert overload here.
Understanding and addressing these ethical issues is essential for fostering a healthcare environment rooted in integrity, compassion, and fairness.





