Mastering Nursing Documentation and Medical Records Management
Accurate and systematic documentation is fundamental to effective nursing practice and patient care continuity. Proper charting not only ensures legal compliance but also enhances communication among healthcare providers, ultimately improving patient outcomes. This guide explores the essentials of nursing charting, the structure of medical records, and best practices for maintaining thorough, organized documentation.
Understanding Medical Records and Charting Systems
Medical records, also known as health records or patient charts, serve as comprehensive repositories of a patient’s medical history, treatments, and healthcare interactions over time. They are vital for tracking disease progression, supporting clinical decisions, and providing legal documentation of care. In recent years, many healthcare facilities have transitioned from traditional paper-based systems to Electronic Health Records (EHRs), which significantly improve access, interoperability, and efficiency. For more insights into evolving healthcare technologies, consider reviewing the latest developments in health insurance offerings.
The setup of medical records varies across institutions, but generally, they follow a structured outline to ensure consistency and completeness. A typical medical record template might include the following sections:
Table: Example of a Medical Record Template
| Section | Content Description |
| — | — |
| Patient Data | Name, age, gender, address, contact details |
| Responsible Provider | Name and contact information of the primary caregiver |
| Insurance Details | Insurance provider, policy number |
| Allergies | Known allergies to medications, foods, or environmental factors |
| Medication Plan | Prescriptions with dosages, frequency, and indications |
| Medical and Family History | Past illnesses, surgeries, hereditary conditions with dates and relations |
| Social History | Lifestyle factors such as smoking, alcohol use, substance intake, occupation, and relationships |
| Visit Documentation | Date, reason for visit, clinical findings, treatments administered |
| Lab and Imaging Results | Test outcomes and imaging reports |
Retention policies for medical records depend on regional regulations, patient age, and record type. Typically, adult records in the US must be stored for at least 6 to 10 years after the last patient interaction. Records for minors should be kept until they reach the age of majority plus the legally mandated retention period. Staying compliant with these standards is crucial for legal and ethical reasons.
Effective Nursing Charting Methods
Nursing charting systems are designed to promote clarity, consistency, and efficiency in documenting patient care. They help nurses maintain organized records that accurately reflect ongoing assessments and interventions. One common approach is focus charting, which emphasizes specific patient problems or care areas. An example of focus charting might include:
Focus: Shortness of breath
Date: [Insert Date]
Interesting:
- Mastering medical management enhancing healthcare operations and outcomes
- Mastering medical documentation essential skills for accurate patient records
- Understanding patient medical records ownership and its significance
- The transformative journey of electronic medical records and their impact on healthcares future
Time: [Insert Time]
Data: The patient reports difficulty breathing since this morning. Oxygen saturation measured at 88% on room air.
Action: Positioned the patient in a high Fowler’s position. Administered 2L oxygen via nasal cannula and provided nebulizer therapy.
Response: Post-intervention, respirations decreased to 18 per minute, and oxygen saturation improved to 94%. The patient verbalized relief, stating, “I can breathe easier now.”
Adopting structured documentation methods like this can greatly improve patient safety and communication among the care team. For a deeper understanding of effective communication strategies, explore essential strategies for mastering communication in healthcare.
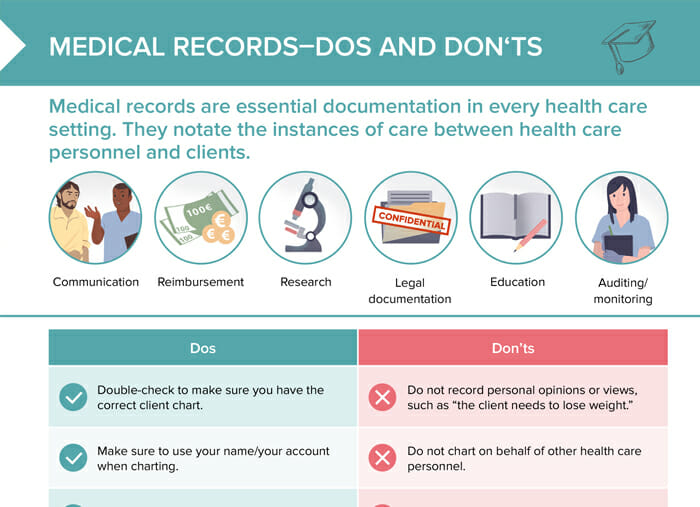
Best Practices for Maintaining Accurate Records
Maintaining high-quality nursing documentation requires attention to detail, consistency, and adherence to legal standards. Some best practices include:
- Use clear, concise language free of abbreviations that may be misunderstood.
- Document objectively, focusing on factual information rather than opinions.
- Record date and time for every entry to establish a precise timeline.
- Sign and authenticate each entry with your full name and credentials.
- Correct errors promptly by drawing a single line through the mistake, noting the correction, and initialing.
- Keep records confidential and secure, following institutional policies and regulations.
With accurate documentation, healthcare providers can better coordinate care, evaluate treatment effectiveness, and meet legal requirements. To improve your communication skills within healthcare settings, review strategies for mastering healthcare communication.
Conclusion
Effective nursing charting and meticulous record-keeping are cornerstones of quality patient care and legal compliance. Embracing structured systems like focus charting, understanding the organization of medical records, and adhering to best practices can significantly enhance your documentation skills. As healthcare continues to evolve, staying informed about new technologies and standards will help you provide the best possible care while ensuring compliance with regulatory requirements. For further insights into healthcare management and policy, explore the latest trends in healthcare service offerings.





