Key Considerations for Implementing Effective Health Information Exchanges
Efficient and secure sharing of health data is transforming the landscape of healthcare delivery. As digital health initiatives expand, understanding the critical factors involved in establishing and operating a successful Health Information Exchange (HIE) becomes essential for providers, policymakers, and stakeholders. This guide explores the core considerations necessary for optimizing HIE systems, emphasizing privacy, interoperability, governance, and future growth opportunities.
Foundations of Health Information Exchange
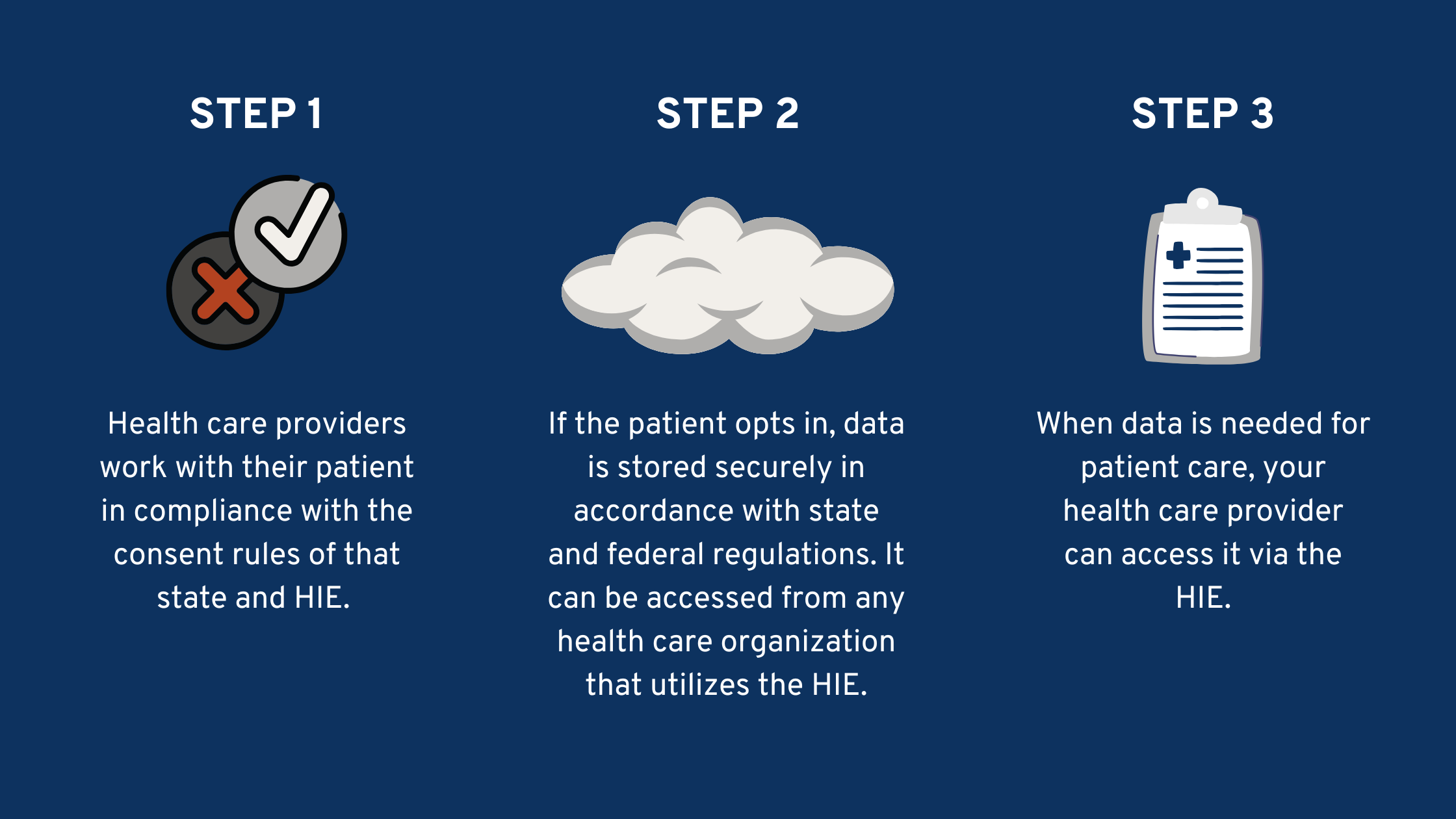
Health Information Exchange (HIE) involves the electronic transfer of patient information across various healthcare organizations, facilitating seamless communication among providers, hospitals, laboratories, and public health agencies. By enabling real-time data sharing, HIEs support clinical decision-making, improve care coordination, and reduce redundant testing. The ultimate goal is to ensure that accurate health data is available when and where it is needed, regardless of the setting or location.
HIE systems operate in accordance with all applicable federal and state data privacy laws, including the Health Insurance Portability and Accountability Act (HIPAA). These regulations specify permissible purposes for data sharing, such as treatment, payment, and healthcare operations, while safeguarding patient privacy and data security. For example, many HIEs connect to electronic health records (EHRs), health systems, and national networks to deliver precise, real-time information at the point of care. When managed responsibly, HIEs support a more interconnected, efficient, and equitable healthcare system.
The Importance of Interoperability and Connectivity
Achieving interoperability is fundamental for effective HIE. It involves adopting standardized data formats and communication protocols, such as HL7 and FHIR, to ensure that diverse systems can exchange information seamlessly. The integration of standards like these underpins the secure and efficient transfer of data across different platforms and organizations.
Many HIEs are linked to national networks, such as the eHealth Exchange or Carequality, which connect local and regional exchanges into a broader, nationwide framework. These shared networks utilize common technology standards and robust privacy safeguards to facilitate data flow across state lines and organizational boundaries. Supporting nationwide interoperability is critical for patient mobility, especially when receiving care across different regions.
One key federal initiative in this space is the Trusted Exchange Framework and Common Agreement (TEFCA). TEFCA aims to unify existing national networks by establishing a common, scalable infrastructure that simplifies the connection process for health data exchange. Although participation in TEFCA is voluntary, many HIEs and healthcare organizations choose to engage directly or through partnerships with Qualified Health Information Networks (QHINs). This initiative reduces fragmentation and fosters a more cohesive health data ecosystem see more about the broad goals of federal interoperability efforts.
Governance, Privacy, and Security Protocols
Strong governance structures are essential for maintaining accountability, transparency, and stakeholder engagement within HIEs. Clear policies on data access, sharing, and use help build trust among participants and patients alike. To comply with privacy laws and protect sensitive information, HIEs implement advanced security measures such as encryption, role-based access controls, and regular security audits.
Adherence to industry standards like HL7 and FHIR promotes interoperability while ensuring data security. Additionally, compliance with HIPAA and other applicable regulations is non-negotiable. Many HIEs also support patient access to their health information through secure portals, enabling individuals to review and manage their records actively. This transparency promotes patient engagement and aligns with the movement toward more patient-centered healthcare.
Interesting:
- Key criteria for effective quality indicator sets a comprehensive review
- Navigating key challenges in engaging stakeholders for health and healthcare guideline development
- Building a data driven future for scotlands health and social care system
- Comprehensive strategies for effective data mapping in healthcare clinics
Patients retain the right to opt out of data sharing through the HIE, which can limit their providers’ ability to access comprehensive health information. The opt-out process typically involves formal requests through the HIE or healthcare providers, and it is vital for patients to understand the implications of their choices. Despite the challenges, balancing privacy with the benefits of data sharing remains a core priority for HIEs.
Expanding Role and Future Directions
While HIEs initially focused on clinical data sharing, their scope is expanding to include public health, social determinants of health, and population health management. Many states are increasingly relying on real-time, comprehensive data to support disease surveillance, health equity initiatives, and crisis response efforts. This evolution has led to the concept of a Health Data Utility (HDU), a trusted, neutral entity responsible for meeting these broader data needs across both public and private sectors.
HIEs are well-positioned to serve as HDUs due to their existing infrastructure, governance, and experience in secure data exchange. They are expanding their capabilities to provide longitudinal, actionable insights that inform care delivery, policy-making, and public health strategies. For example, understanding how data mining techniques are used in healthcare can enhance predictive analytics and early intervention efforts see how data mining is applied in health.
Despite their advantages, HIEs face challenges such as protecting sensitive data, overcoming technical and regulatory barriers, and ensuring sustainable funding. Many rely on a mix of federal grants, state funds, and provider fees, which can be uncertain. Continued innovation and collaboration are necessary to address these issues and realize the full potential of health data exchange.
Critical Success Factors for Implementation
Implementing an effective HIE requires careful planning around technical infrastructure, stakeholder engagement, and compliance. Key considerations include:
- Establishing clear governance policies that define roles, responsibilities, and data-sharing agreements.
- Ensuring robust cybersecurity measures to safeguard health information during transmission and storage.
- Promoting stakeholder collaboration among hospitals, clinics, public health agencies, and community organizations to foster trust.
- Adopting standardized data formats to facilitate interoperability and reduce data silos.
- Providing training and support to providers and staff to encourage adoption and effective use of HIE systems.
- Developing sustainability models that diversify revenue streams beyond initial grants or funding sources.
Furthermore, ensuring equitable access to HIE benefits involves engaging underserved populations and addressing social determinants of health. By doing so, HIEs can help reduce disparities and promote health equity across communities.
Conclusion
Health Information Exchange is a vital component of modern healthcare, offering numerous benefits from improved care coordination to enhanced public health surveillance. As technology advances and data needs grow, stakeholders must prioritize privacy, interoperability, governance, and sustainability to maximize these advantages. The continuous evolution of HIEs, supported by initiatives like TEFCA, promises a future where health data flows seamlessly and securely across all levels of care, ultimately leading to better health outcomes for everyone.





