Examining the Benefits and Drawbacks of Universal Healthcare in 2025
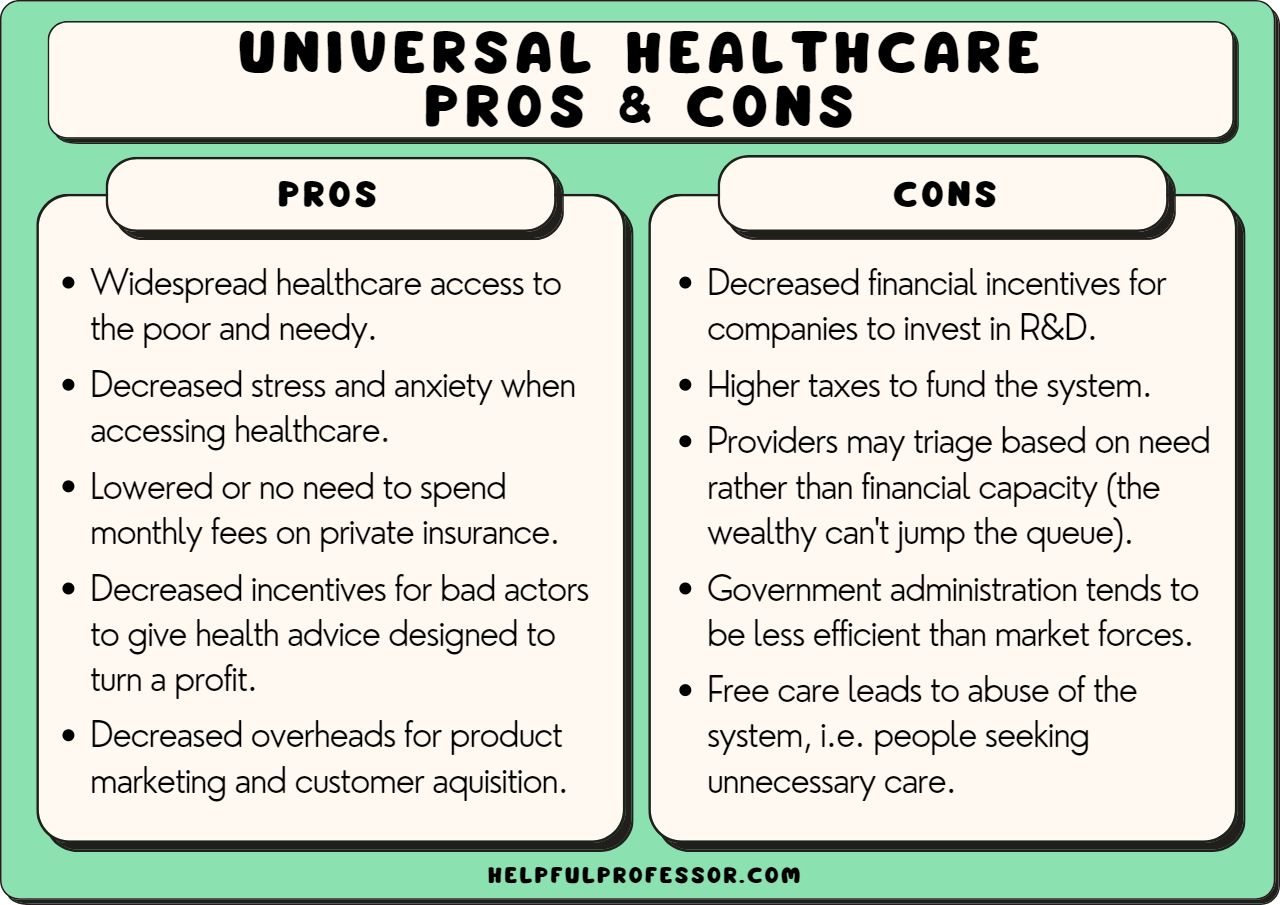
Universal healthcare remains a highly debated topic worldwide, offering numerous advantages such as reduced costs and increased access, while also facing criticism over potential inefficiencies and quality concerns. Understanding the complex landscape of this system requires a nuanced look at its pros and cons, recognizing that many of these points depend heavily on implementation and context. This discussion explores the various facets of universal health coverage, providing insights into its potential impacts on society, the economy, and individual well-being.
Many advocates argue that universal health care leads to fewer administrative expenses, broader accessibility, and improved health outcomes. Conversely, critics highlight issues like government expenditure growth, bureaucratic bloat, and possible declines in care quality. This balanced perspective aims to inform policymakers, healthcare professionals, and the public about the multifaceted nature of adopting such a system.
Pros and Cons of Universal Health Care
Pro 1: Reduced Overall Healthcare Expenses
While research into the financial implications of universal healthcare yields mixed results, some studies suggest that costs tend to be lower under a universal model. For instance, research by Galvani and Fitzpatrick (2020) indicates that a dollar spent within a universal system often yields more value than in a privatized framework. This efficiency stems from decreased transaction costs and minimized profit margins that typically inflate private healthcare spending.
In private or semi-private systems, the involvement of numerous profit-driven entities increases expenses due to administrative overheads and profit margins. By contrast, a government-managed system can streamline logistics and eliminate the need for profit-based costs, leading to potentially significant savings. Although some private sector involvement may persist, most services are managed publicly, enabling centralized pricing and reducing unnecessary expenditure. For more on how AI is transforming healthcare efficiency, see this comprehensive guide.
Pro 2: Streamlined Administrative Processes
The administration of healthcare in systems with multiple insurers and providers can become extraordinarily complicated, often requiring extensive bureaucratic infrastructure. This complexity raises operational costs without necessarily improving patient care quality. Under a universal program, a single payer—typically the government—simplifies these processes by establishing uniform rules and reducing administrative burdens.
Even if private hospitals continue to operate, billing directly to the government rather than multiple insurance companies significantly cuts down on paperwork and administrative costs. This simplification can free up resources and reduce overhead, ostensibly leading to a leaner system. However, debates persist about whether bureaucracy actually diminishes, as some argue that large government agencies can become inefficient. For a detailed look at different healthcare systems, including Canada’s model, visit this resource.
Pro 3: Longer Life Expectancy
Numerous studies associate universal healthcare with increased longevity, including research by Ranhabat et al. (2018). Countries with comprehensive government-funded care tend to see higher overall life expectancy, partly because preventive care and early intervention are more accessible. Early treatment and regular screenings help manage chronic conditions and reduce the incidence of severe health crises in later years.
This preventive approach not only extends lifespan but also enhances quality of life in old age. Early access to health services can mitigate long-term health issues, resulting in healthier aging populations. To explore how technology influences healthcare accessibility, see this article.
Pro 4: Economic Benefits
A universal health care system can positively influence a nation’s economy through various channels. A healthier workforce tends to be more productive, with fewer sick days and longer working lives. Additionally, universal coverage can create stable employment opportunities in healthcare administration, public health, and related sectors, even during economic downturns.
Government-led healthcare spending can also be more flexible, allowing for strategic investments and stimulus measures. However, some argue that the sizable private healthcare industry in countries like the USA might contract if universal models are adopted, which could impact existing employment. For insights into healthcare’s role in economic growth, see this analysis.
Pro 5: Fostering Innovation and Data Sharing
In a universal system, data can be more freely shared and utilized for research and development without the constraints of proprietary protections. This openness can accelerate medical discoveries and improve patient care. Clinicians and researchers can access vast pools of anonymized data, facilitating the development of new treatments and personalized medicine.
While some contend that profit motives drive innovation in private healthcare, a publicly funded system can prioritize public health benefits over profit. Moreover, open data policies can foster collaboration and technological advancements. For a broader understanding of digital health innovations, see this resource.
Pro 6: Improved Quality of Life
Universal healthcare encourages early diagnosis and treatment, which can significantly improve individual health outcomes. When financial barriers are removed, people are more likely to seek care promptly, reducing the severity of illnesses and preventing complications. Consequently, populations tend to enjoy longer, healthier, and more active lives.
Healthier individuals not only experience better personal well-being but also contribute positively to their communities and the economy. This proactive approach often results in fewer long-term medical conditions and enhances overall happiness. To understand mobile health services’ role in expanding access, see this article.
Pro 7: Equitable Access for All
A key advantage of a unified healthcare system is its potential to promote fairness. Regardless of socioeconomic status or geographical location, everyone can access essential health services. This standardization reduces disparities caused by income inequality or regional healthcare quality differences, ensuring that vulnerable populations are not left behind.
In such systems, even those in remote or underserved areas receive essential care, contributing to overall societal well-being and social cohesion. For more on how universal coverage addresses inequalities, visit this resource.
Pro 8: Long-Term Investment in Society
While increased healthcare spending in the short term can seem burdensome, long-term savings often offset these costs. Preventative care can detect health issues early, avoiding expensive treatments later. For example, early detection of cancer or managing chronic diseases effectively reduces the need for costly emergency interventions.
Investing in healthcare can also reduce societal costs associated with disability, unemployment, and social care for aging populations. This proactive approach fosters a healthier, more productive society over time. To explore how mobile healthcare aims to improve service delivery, see this article.
Pro 9: Reduced Stress and Financial Anxiety
Financial concerns are a major source of stress for many individuals facing health issues. A universal system alleviates this burden by eliminating or reducing out-of-pocket expenses for medical care. This security encourages people to seek urgent care without fear of crippling bills or bankruptcy.
Personal experiences from countries with universal health coverage often highlight the peace of mind that comes with knowing healthcare costs are covered. This mental relief can significantly improve overall well-being and societal health. For insights on data security and patient trust, see this article.
Pro 10: Upholding Human Rights
Access to healthcare is widely recognized as a fundamental human right, enshrined in declarations by the United Nations and the World Health Organization. Implementing universal coverage ensures no one is excluded from essential health services due to financial limitations, promoting social justice and equality.
A government commitment to universal health care demonstrates respect for human dignity and collective responsibility. This approach underscores the importance of health as a shared societal asset rather than a privilege for the few. To learn more about mobile healthcare’s role in human rights, see this resource.
Pro 11: Encouraging Entrepreneurial Opportunities
Interestingly, shifting healthcare from private to public domains can stimulate entrepreneurship in other areas. In countries like the USA, individuals leaving employment to start their own businesses often face losing employer-sponsored health insurance, which can be prohibitively expensive otherwise.
A universal system could reduce this barrier, enabling more people to pursue innovative ventures without fear of losing essential coverage. This environment could foster new health technologies, services, and startups aligned with public health goals. For perspectives on AI in healthcare, see this article.
Interesting:
- Understanding the role and benefits of clinically integrated networks in healthcare
- The significance of hipaa key benefits and its role in modern healthcare
- Navigating the benefits and challenges of ai in healthcare a comprehensive review
- Navigating the impact of artificial intelligence in healthcare benefits challenges and future directions
Cons and Challenges of Universal Health Care
Con 1: Escalating Government Spending
Public healthcare systems often experience cost overruns, especially as new, expensive treatments and medications emerge. This trend can lead to rapidly increasing government expenditure, raising concerns about fiscal sustainability. As healthcare costs grow, governments may face pressure to raise taxes or cut other vital services, risking economic stability.
Overutilization, driven by the absence of user fees, can further inflate costs, straining public budgets. Managing these financial pressures remains a central challenge for universal healthcare models. For more on health system financing, see this resource.
Con 2: Bureaucratic Inefficiency
Large-scale government programs are often criticized for their bureaucratic complexity. Excessive regulations, paperwork, and administrative layers can slow decision-making and waste resources. This inefficiency can diminish the quality of care and frustrate both providers and patients.
While some argue that private healthcare also suffers from bureaucratic issues, government-run systems tend to be more prone to red tape due to their scale and political influences. For a comparative analysis of healthcare governance, visit this article.
Con 3: Potential Decline in Care Quality
Despite the promise of universal healthcare, some systems struggle with long wait times and rationing, especially when resources are limited. This can result in delayed treatments and reduced access to the latest medical innovations. Critics argue that a one-size-fits-all approach might lower the quality of care compared to private systems where patients can pay for faster or more specialized services.
Furthermore, budget constraints may force governments to limit certain procedures or treatments, impacting patient outcomes. For insights into how some universal systems manage care, see this resource.
Con 4: Brain Drain of Medical Professionals
Lower salaries and limited opportunities for specialization can make universal healthcare countries less attractive to top-tier medical professionals. This can lead to a phenomenon known as “brain drain,” where skilled healthcare workers emigrate to countries with higher pay and better working conditions, such as from Canada to the US.
This migration exacerbates staffing shortages and can compromise the quality of care in the home country. For more on workforce challenges, see this article.
Con 5: Reduced Incentive for Innovation
Without the profit motive, private companies often drive the development of new drugs and medical technologies. A purely public system may lack sufficient financial incentives to pursue groundbreaking research, potentially slowing innovation. This could delay the introduction of advanced treatments and limit the availability of cutting-edge medical solutions.
While public funding can support research, the absence of competitive pressures might diminish the pace of medical progress. For further insights, see this article.
Con 6: Risk Compensation Behavior
Knowing that healthcare costs are covered regardless of personal behavior may lead some individuals to neglect health precautions, engaging in riskier activities or ignoring early symptoms. This complacency can increase the frequency of preventable health issues, raising overall system costs.
Such moral hazard concerns are debated, but evidence suggests that behavioral changes can influence healthcare utilization in universal systems. For more on the importance of data security in healthcare, see this resource.
Con 7: Higher Tax Burden
Funding universal health coverage typically requires increased taxation, which can be politically sensitive. Countries like Australia have implemented higher taxes to support their systems, and debates over tax hikes often hinder reforms in other nations, including the US.
Balancing funding needs with public acceptance remains a significant obstacle. For a detailed comparison of healthcare financing models, see this article.
Con 8: Corruption and Resource Waste
Large government programs are susceptible to mismanagement and corruption, which can divert resources away from patient care. Wasteful spending, favoritism, and lack of transparency can undermine public trust and reduce the system’s efficiency.
Ensuring accountability and oversight is essential to prevent these issues and maintain system integrity. To explore how digital tools can enhance healthcare security, see this article.
Con 9: Political and Industry Opposition
Implementing universal healthcare often faces fierce resistance from powerful interest groups, including insurance companies, pharmaceutical firms, and medical associations. These entities may oppose reforms that threaten their profits or market influence, leading to legislative gridlock and public opposition.
Overcoming such opposition requires strategic policymaking and stakeholder engagement to align interests. For insights into the influence of industry on healthcare policies, see this resource.
Con 10: Limitations on Personal Freedoms
Mandatory participation in a universal healthcare system, funded through taxes or premiums, can be viewed as infringing on individual liberties. Critics argue that voluntary models better preserve personal choice, whereas compulsory coverage can feel coercive.
Balancing collective health needs with personal freedoms remains a contentious aspect of healthcare reform debates. For more on digital health and privacy rights, see this article.
Conclusion
The debate over universal healthcare involves weighing its potential to promote health equity, economic stability, and societal well-being against concerns about costs, efficiency, and personal freedoms. The effectiveness of such a system largely depends on careful planning, transparent management, and continuous evaluation. As healthcare continues to evolve, understanding both sides of the argument is essential for making informed decisions that serve the best interests of society.
References
Galvani, A. P., & Fitzpatrick, M. C. (2020). Cost-effectiveness of transitional US plans for universal health care. The Lancet, 395(10238), 1692-1693.
Rashford, M. (2007, January). A universal healthcare system: is it right for the United States?. In Nursing Forum (Vol. 42, No. 1, pp. 3-11). Malden, USA: Blackwell Publishing Inc.
Ranabhat, C. L., Atkinson, J., Park, M. B., Kim, C. B., & Jakovljevic, M. (2018). The influence of universal health coverage on life expectancy at birth (LEAB) and healthy life expectancy (HALE): a multi-country cross-sectional study. Frontiers in pharmacology, 9, 960. Doi: https://doi.org/10.3389%2Ffphar.2018.00960





