The persistent disparities in healthcare access across rural regions pose significant challenges worldwide, including in Hungary. To address these issues, innovative solutions like mobile telemedicine units have emerged as promising strategies to bridge the healthcare gap, improve outcomes, and foster equitable health services. This comprehensive study explores a pioneering nationwide telemedicine initiative that leverages specialized mobile clinics to deliver both primary and specialist care directly to underserved populations, demonstrating the potential to transform rural healthcare delivery.
Introduction
Digital health technologies have revolutionized the way medical services are delivered, encompassing mobile health (mHealth), electronic health (eHealth), and advanced information science applications such as artificial intelligence and big data analytics. The evolution of broadband internet and digital networks globally has facilitated remarkable improvements in telemedicine, which the WHO defines as “the use of information and communication technologies to improve patient outcomes by increasing access to care and medical information.” Similarly, telehealth involves delivering healthcare services remotely through telecommunications and virtual tools, often used synonymously in medical practice.
In rural and remote areas, where healthcare deserts are common, telemedicine plays a vital role in overcoming geographical barriers and providing access to both primary and specialized healthcare services. These regions often suffer from shortages of qualified providers, higher chronic disease prevalence, and poorer health outcomes compared to urban centers. Mobile health clinics, such as specially equipped vehicles traveling directly into communities, have shown promising results in delivering preventive and primary care, especially in settings where conventional infrastructure is lacking. For example, a study in the United States indicated that mobile health units can effectively replace some institutional services, offering a cost-effective alternative for rural populations.
The broader application of telemedicine encompasses various disciplines, including teleradiology, telecardiology, teledermatology, and telepsychiatry, each contributing to comprehensive chronic disease management. Early studies highlight the benefits of remote monitoring devices, which provide continuous data on vital signs and health parameters, improving disease control and patient engagement. For instance, telemonitoring of diabetic patients has been associated with better glycemic control and reduced systolic blood pressure, supporting the integration of digital tools into routine care.
However, challenges such as digital literacy, infrastructural limitations, and regulatory barriers continue to hinder widespread implementation, particularly in low-income or geographically isolated regions. Many telemedicine workflows rely heavily on self-reported data, which may be less reliable than professionally collected information, emphasizing the need for structured protocols and well-trained personnel. Moreover, the cost of deploying sophisticated digital infrastructure can be significant, requiring careful economic analyses to ensure sustainability.
In Hungary, healthcare disparities are evident across geographic and socio-economic divides. Segregated communities tend to utilize healthcare services more frequently but receive disproportionately lower-quality care, contributing to higher premature mortality rates. Recognizing these inequalities, the Hungarian government launched a comprehensive socioeconomic development program in 2019 targeting the country’s most disadvantaged rural settlements, known as “FeTe” villages. This initiative aims to improve living conditions and healthcare access in these areas, which are characterized by poor housing, limited education, and high birth rates.
Aligned with this national strategy, research collaborations between the Hungarian Charity Service of the Order of Malta and academic institutions have led to the development of a novel mobile healthcare ecosystem. This system consists of motorized units equipped with advanced telemedicine devices, point-of-care testing (POCT) tools, and audiovisual platforms, designed to reach populations in remote villages. The overarching goal is to deliver both general and specialist care directly to underserved regions, democratizing access and reducing health disparities. This approach, unprecedented on a global scale, integrates logistics, data collection, and clinical support under professional supervision to ensure reliable care delivery.
Materials and Methods
Study Design
This prospective observational pilot study evaluates the feasibility, cost-effectiveness, and health impact of deploying mobile telemedicine units across five rural districts in Hungary over a six-month period (April–October 2023). The intervention was tailored to local needs, emphasizing practicality and responsiveness rather than strict adherence to predefined telemedicine frameworks. The study targeted communities within the 300 designated FeTe settlements, which were selected based on socioeconomic disadvantage, ensuring the intervention reached populations most in need.
The mobile units were operated from a centralized base in central Hungary, with each vehicle traveling approximately 500 km daily to reach distant villages, often facing logistical challenges such as variable internet connectivity and rough roads. To ensure system reliability, special precautions were taken to protect sensitive medical devices from vibrations, moisture, and temperature fluctuations during transportation.
Study Area Description
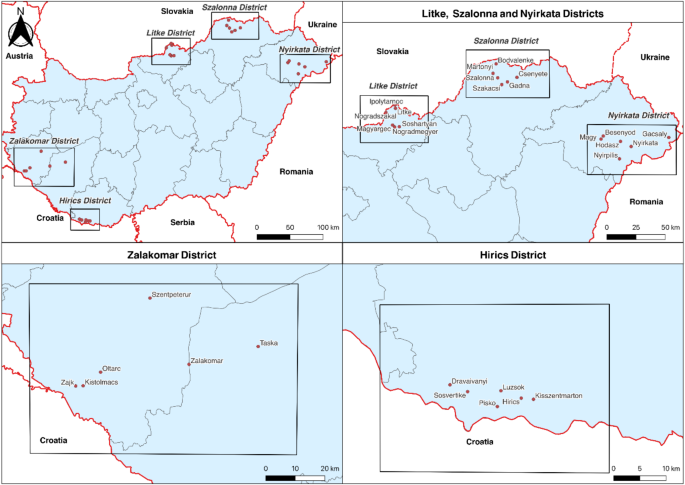
The intervention involved five districts—Zalakomar, Hirics, Litke, Szalonna, and Nyirkata—serving a total population of 21,477 residents according to the 2022 census. These districts were selected because of their high levels of socioeconomic deprivation and limited healthcare infrastructure. In comparison, control settlements with similar geographical and demographic characteristics but without access to mobile healthcare units were identified, totaling a population of over 200,000 across 171 locations.
Demographic analysis revealed significant differences: the age structure skewed younger in the intervention areas, with higher birth rates and lower life expectancy than national averages. Socioeconomic factors, such as education levels and Roma population proportions, indicated higher levels of poverty and lower educational attainment, underscoring the necessity for targeted healthcare interventions.
The Mobile Healthcare Service Centers
The core of the project involved 12 specialized mobile clinics based on Fiat Ducato Maxi vehicles, each fitted with power generators, telemedicine systems, POCT devices, and audiovisual equipment. These vehicles facilitated two tiers of services:
- Basic medical support: conducted by nurses and GPs through physical examinations and teleconsultations.
- Specialist care: delivered remotely by specialists in cardiology, dermatology, pulmonology, and endocrinology, based on initial assessments.
Connectivity challenges were managed through partnerships with multiple internet providers, ensuring at least minimal bandwidth for video and data transmission. The telemedicine setup included cameras, portable ECGs, spirometers, blood analyzers, and other diagnostic tools, all integrated with a secure software platform for data management and remote consultation.
Telemedical Intervention
The intervention encompassed community health education, chronic disease screening, acute and long-term care, and diagnostic referrals. Preventive activities included health forums and targeted screening for hypertension, diabetes, and other risk factors. Patients received tailored counseling, and follow-up plans were established for chronic cases. The system facilitated real-time consultations with specialists, enabling timely diagnosis and management.
Cost Analysis
The economic evaluation utilized national healthcare expenditure data from the Hungarian National Health Insurance Fund to estimate per capita spending in primary care settings. Costs associated with operating the mobile units—including staff salaries, test consumables, vehicle maintenance, and IT infrastructure—were analyzed and compared to existing healthcare budgets. The financial analysis aimed to determine the sustainability and scalability of this telemedicine approach, considering the current underfunding of rural primary care practices.
Interesting:
- Enhancing primary healthcare in rural areas a comprehensive scoping review of interventions
- Enhancing healthcare quality through incentive programs in california
- Effective strategies for measuring and enhancing patient satisfaction in healthcare
- Enhancing healthcare through effective clinical documentation improvement
- Understanding the role of managed service providers in healthcare and when to seek better solutions
User Feedback and Data Collection
Structured questionnaires captured patient and provider satisfaction, focusing on the quality of care, interaction experience, and willingness to continue using telemedicine services. Data collection included demographic variables, health parameters, referral rates, and health behaviors like smoking and alcohol consumption. Statistical analyses employed non-parametric tests to account for data distribution, with adjustments made for socio-economic factors.
Ethical Considerations
The study received approval from the Hungarian Medical Research Council (ETT–TUKEB), with strict adherence to GDPR and data privacy standards. All patient information was anonymized, with informed consent obtained prior to participation. Secure encryption protocols protected communication channels and data storage.
Results
Population Characteristics
The intervention areas exhibited a younger demographic, higher birth rates, and lower life expectancy compared to national data, with notable socioeconomic disadvantages such as elevated Roma populations and lower educational levels. These factors contributed to increased healthcare needs and underscored the importance of targeted mobile interventions.
Healthcare Services Delivered
Over six months, 1,889 individuals were examined across 770 consultation days, with 4,118 telemedicine events conducted—averaging approximately 2.44 per adult and 1.36 per child. The services included screenings, chronic care management, laboratory diagnostics, and referrals. Notably, 105 new hypertension and 26 new diabetes cases were diagnosed, demonstrating the system’s capacity for early detection.
Referral activity was significant: 987 patients received referrals, with a notable 10% reduction in the relative rate of external healthcare referrals compared to control regions, suggesting that the telemedicine system effectively alleviated pressure on local hospitals and clinics. Patient satisfaction was high, with over 96% expressing full satisfaction and willingness to recommend the services.
Use of Telemedical Devices
Devices such as electronic stethoscopes and portable ECGs were heavily utilized, supporting diagnostic accuracy. POCT devices performed blood analyses, urine tests, and other rapid diagnostics, facilitating timely clinical decisions. The most frequent tests included blood sampling, HbA1c, and urine analysis, which underpin the system’s diagnostic robustness.
Health Outcomes and Behaviors
Screenings identified numerous new cases of hypertension and diabetes, and assessments of lifestyle factors revealed higher-than-average smoking and alcohol consumption rates, emphasizing the need for health promotion activities. The intervention also documented a high prevalence of overweight and obesity, correlating with risk factors for chronic diseases.
Economic Analysis
Operating costs for the telemedicine units exceeded the current primary care budgets allocated to rural areas, highlighting the financial challenges of scaling such programs. Nonetheless, the potential reduction in unnecessary hospital referrals and improved disease detection suggest long-term cost savings and health benefits.
Discussion
The deployment of mobile telemedicine units in Hungary demonstrates a promising approach to bridging healthcare disparities in rural communities. The system’s ability to deliver primary and specialist care directly to underserved populations resulted in early disease detection, reduced referral rates, and high patient and provider satisfaction. The innovative integration of diagnostic tools and teleconsultation platforms provides a scalable model adaptable to other regions facing similar challenges.
While initial results are encouraging, limitations include the short duration of the pilot, which constrains the assessment of long-term health outcomes. Infrastructure challenges, such as unreliable internet connectivity and limited digital literacy, must be addressed to optimize system performance. Future efforts should focus on expanding diagnostic capabilities, enhancing training, and conducting comprehensive cost-effectiveness analyses to ensure sustainability.
This initiative underscores the critical importance of strategic investments in digital infrastructure and workforce development. The success of such telemedicine programs relies on coordinated efforts between policymakers, healthcare providers, and technology developers. By continuously refining these systems, Hungary can establish a sustainable model that significantly reduces health disparities and improves chronic disease management in rural areas. For further guidance on protecting patient information, see securing healthcare data in the digital age, and for strategies to enhance data management integrity, visit ensuring integrity and confidentiality in healthcare data management.
Conclusion
Mobile telemedicine clinics equipped with advanced diagnostic and communication technology offer a compelling solution to improve healthcare access in rural and underserved regions. This pilot project in Hungary demonstrates the feasibility, acceptability, and potential health benefits of deploying such systems at a national scale. High satisfaction levels, effective early detection of chronic diseases, and reductions in unnecessary referrals highlight the transformative potential of telemedicine in bridging healthcare gaps. Addressing infrastructural and technological barriers, alongside ongoing evaluation of long-term outcomes, will be essential to establish sustainable, scalable models for rural healthcare improvement.
Data availability
The datasets generated and analyzed during this study are available from the corresponding author upon reasonable request, respecting privacy and ethical considerations. Interested researchers may contact Dr. János Sándor at janos.sandor@med.unideb.hu to obtain access for scholarly purposes.
—
This work underscores the importance of innovative, technology-driven solutions in transforming healthcare delivery for marginalized populations, supporting global efforts toward health equity.